Article by Dr. Clarence Tam HBSc, DDS, FIADFE, AAACD
A CHAMELEON SUPERCOMPOSITE
INTRODUCTION
The name of the game in modern-day esthetic and restorative dentistry is that of Responsible Esthetics. The goal of treatment typically strives to correct any structural and cosmetic shortfalls in both biologically-driven and trauma-affected teeth with the precise, artistic placement of various replacement layers, all whilst respecting and retaining a maximal volume of residual tooth structure. Anterior teeth can be affected by enamel and dentin dysplasia, caries and sclerotic conditions and are characterized by a laundry list of genetically-derived and environmentally-acquired conditions with an esthetic deficit that often threaten an individual’s functional and psychosocial integrity if not restored to the seamless picture of health.
Missing and defective tooth structure must be categorized into its attendant enamel and dentin components. Both substrates are distinctly different in composition, with enamel being highly inorganic in nature and dentin proportionately more collagenous in nature. The latter stratum is responsible for the refraction of light, the expression of the true color of the tooth, namely the hue and the endowment of fracture toughness or resilience in functional performance. The value and chroma are the other elements of color and are modified by the thickness of enamel. The replacement of enamel has been found to be best substituted from a biomechanical perspective by adhesively-bonded indirect porcelain restorations, and dentin using both composite resin and short fiber reinforced composite (SFRC), the latter imparting increased fracture toughness in large volume replacement restorations, especially those with pericervical structural deficits.
In adolescent patients, the gold standard of treatment involves direct composite resin, as often zero to minimal tooth structure preparation is required as a foundation to the bonded restorative. It would be impractical to use bonded indirect restorations when the development of the dentition in puberty is continuous, especially with the retraction of gingiva as one progresses to young adulthood. Resin composite allows prescience in the opportunity to predictably modify and/or add to the existing restoration if dental bleaching for the other teeth is desired or if a further traumatic incident is encountered. The ability to modify bonded porcelain is not predictable and frequent marginal failures occur due to a lower shear bond strength to bonded composite, especially after thermocycling. This is despite our ability to establish a chemical linkage via silane coupling agents from silicate ceramics to resin composite especially at a blended interface.
STATEMENT OF PROBLEM
Dental shades in clinical dentistry have long been classified using the VITA* Classical A1 – D4 shade guide. Despite being ubiquitous in dental practices, composite resin systems with corresponding shade systems do not satisfactorily match to their purported shade1. Floriani et al found that various mixtures of different shades in one system was required to achieve an acceptable color match with the VITA* Classical shades using the CIEDE2000 formula. Testing another composite resin, they found that none of the A1, A2 or A3 shades matched acceptably to the standard shade guide2. Indeed, even with indirect ceramic layering systems, a wide range of unacceptable discrepancy was noted between VITA* labeled porcelain shades and the actual shade guide3. The VITA* Classical shade guide became the standard in dental shade classification with the release of its A1-D4 shade guide in 1985. The majority of human-tested dental shades has been found to be in the A-family (78.5%), followed by C (13.2%), D (5.2%) and B (3.1%)1. As such, the shade accuracy of a given composite system must be important if they are to be visually naturomimetic.
CHAMELEON EFFECT DEVELOPMENT
There are myriad composite resin systems featuring a simplified shade Universal system that have acceptable chameleon effects due to their balance of translucency, light transmission, diffusion and refractive index properties. There is a concern over how these optical properties may change after both thermocycling and wet storage, potentially compromising the excellent initial esthetic blend4. Refractive index (RI) is best optimized when the RI of the inorganic fillers match closely with the RI of the cured organic matrix, typically in a range between 1.47 and 1.525. If the match is dissimilar, this drives up the opacity of the restoration due to heightened refraction and reflection at the filler/matrix interface6.
Layering of composite to mask an intraoral defect is complicated by the need to mask any linear defects such as fracture lines superimposed over the shadowing of the dark intraoral cavity in addition to regional color variations. It is confounded by the requirement to recreate natural maverick and translucent effects particularly in the incisal window region of upper and lower incisors and canines, giving the illusion of a virgin, healthy tooth. This has been historically difficult to accomplish in anterior teeth given the need to block out restorative interfaces with natural tooth structure and recreate a seamless internal structure and details. This detailed layer belies a well contoured enamel layer with realistic translucency, polishability and accurate primary and secondary anatomy.
Adding to the complexities described above, the histoanatomical approach to composite layering dictates that missing enamel is replaced by enamel shades, and dentin by the corresponding dentin shade in the appropriate shade. This shade must be selected at the very start of the appointment, as often even a minute of dehydration has a negative effect on both the perceptibility threshold and acceptability threshold of teeth7, resulting in the incorrect shade.
DEVELOPMENT
CLEARFIL MAJESTY™ ES-2 is a value-based super-nanofilled composite system that covers 15 VITA* shades in just 4 shade options with its Universal series. This Universal series provides a chameleon effect and has 4 variants: Universal (U), Universal Light (UL), Universal Dark (UD) and Universal White (UW). It is the VITA*-approved shading concept relative to color accuracy. Incorporating nano-fillers that consist of silanated barium glass fillers and slanted silica nanoclusters, its wear resistance is high and features minimal abrasiveness against the functional antagonist. The RI of both inorganic filler and organic matrix are well-matched, and the high refractive index of the composite mimics and is extremely similar to natural enamel (1.613) and dentin (1.540), thanks to an innovation labeled Light Diffusion Technology (LDT), which distorts light in a similar way dental tissue does8. There is comfort that the stability of refractive index and other optical transmission properties remains statistically stable even after artificial thermocycling and water-storage aging studies4. The color stability of CLEARFIL MAJESTY™ ES-2 has been proven over time, where a direct comparison to Filtek Ultimate showed CLEARFIL MAJESTY™ ES-2 to feature significantly less color variation from baseline and marginal functional wear over a three to four year period in teeth featuring amelogenesis imperfecta9. This color substantivity is important as dietary and environmental stressors applied over time should have as minimal effect on the restoration to ensure continued esthetic integration.
CLINICAL PROTOCOL
CLEARFIL MAJESTY™ ES-2 Universal is a monochromatic solution that covers the five key shades featured in the CLEARFIL MAJESTY™ ES-2 Premium. As such, it exhibits the most significant LDT relative to all five shades, as its ability is equal when blending to higher value translucent shades as it does to cervical chromatic shades. In a Class IV restoration with a defined fracture line, the challenge is to restore the tooth in a minimal volume of available space. The alchemy requires a complete visual occlusion of the fracture line position, and recreation of internal and external opaque and translucent anatomy along with maverick staining, craze lines and effects. In anterior teeth, the idiom of “the less you see, the less you notice” is not true, especially due to the presence of incisal edge window effects as above, however, materials with the best light diffusion and structure transference properties should be utilized to ensure the highest probability of success.
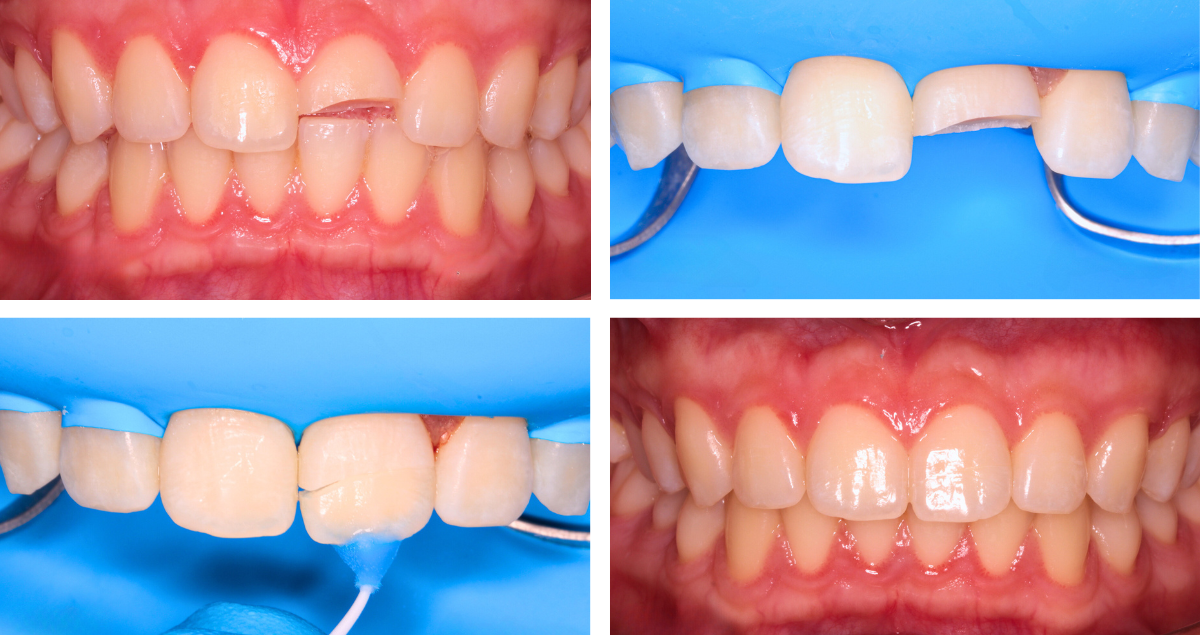
A 15 year old ASA I female presented to the practice exhibiting aged, chromatic composite restorations with poor marginal integration and gross axial overhangs; essentially a gross failure of primary anatomy and esthetics. She had been involved in a bike accident where she high-sided off braking sharply in a face-meets-concrete scenario, resulting in an uncomplicated moderate enamel-dentin fracture with blushing, affecting both the facial and palatal aspects of tooth 1.1 and a mild uncomplicated enamel dentin fracture affecting the distoincisobuccolingual aspect of tooth 2.1. The restoration overhangs were significant, extending into the proximal contour zone, thus obviating effective interdental cleaning. Vitality tests were confirmed along with radiographs to exclude the presence of apical pathology. The patient accepted the option of pre-prosthetic whitening, to improve the value characteristics of the adjacent teeth, allowing the selection of a brighter value shade combination. Intraoral digital scans were acquired and custom bleaching trays with a no reservoir, cervical seal-priority design were fabricated. The patient was instructed to bleach overnight for a 2 week period using a 10% carbamide peroxide solution (Opalesence, Ultradent Products, UT) until her maximal value was reached. Her baseline shade of the incisors was a 1M1/2M1 combination in the upper incisors and a 2M1 in the lower incisors. On final post-bleach assessment she exhibited a lightened shade of VITA* 0M3 in all incisors. The patient was instructed to use a fluoride-containing, amorphous calcium phosphate complex (ToothMousse Plus, GC America) during the following 2 weeks after cessation of whitening whilst the residual oxygen radical species dissipated from the teeth.
Fig. 1. Pre-operative unrestricted smile 1:2 ratio view, teeth 1.1 and 2.1 with old, defective composite restorations with excessive chroma.
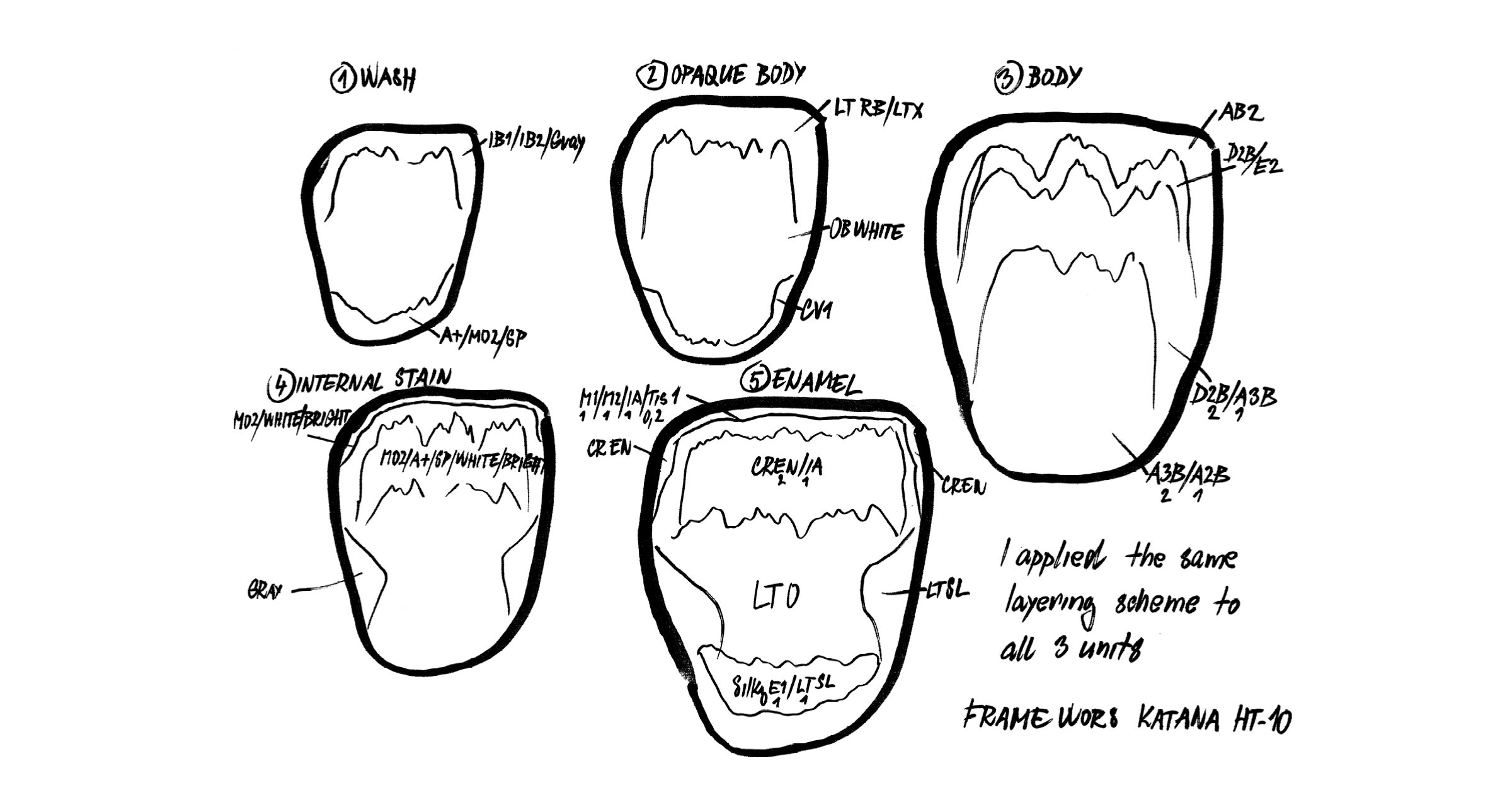
On the day of the procedure, the pre-dehydrated shade was assessed using the supplied “real composite” shade guide tabs featured in the CLEARFIL MAJESTY™ ES-2 Premium system, with the enamel shade being WE (White Enamel) and the dentin shade WD (White Dentin). It was assessed that both white maverick effects as well as a moderate halo effect was desired along with moderate to strong translucency in the incisal window.
The patient was anesthetized using 1.5 carpules of 2% Lignocaine with 1:100,000 epinephrine (Septodont) before a rubber affixed with individual ties for the central incisors (NicTone Medium). Excavation of the old restorative material was undertaken, and the residual natural incisal edge was found to be undermined by a through-and-through fracture. Thus, the preparation was converted into a true Class IV design, with the facioincisal cavosurface margin subjected to an infinity bevel. The maxillary central incisors were isolated from the lateral incisors by way of a serrated metal strip (Komet) and the prepared surfaces subjected to micro particle abrasion using a 29 micron aluminum oxide powder in 17.5% ethanol carrier (Aquacare). The surfaces were subsequently treated with a calcium sodium phosphosilicate powder (Sylc, Aquacare) to increase the inorganic content of the prepared surface especially extending into the exposed tubules. The teeth were etched using a 33% orthophosphoric acid before a 1 minute 2% chlorhexidine scrub (Vista Products). The surface was reduced to a moist dentin surface before the bond applied, air thinned and cured.
A Mylar strip was pre-crimped in the palatoproximal line angles and positioned on the linguoaxial surface of both teeth 1.1 and 2.1. There is no shade guide for the CLEARFIL MAJESTY™ ES-2 Universal U shade, as it bears a significant chameleon effect however it does come in a light (L) and dark (D) variant. The UL shade was deemed the most suitable for the palatal or lingual shelf, with an average thickness of 0.3mm. This layer was applied in a freehand fashion with a focus on establishing the desired outline form of the tooth relative to the contralateral 2.1. The Mylar matrix setup was removed and a precurved metal matrix (Garrison Slickband, Garrison Dental) was oriented in a position perpendicular to its normal placement interproximally, and the end of the curved band tucked into the sulcus before being secured by a wedge. In this way, there is light separation of the central incisors and an intimate contact between the matrix band and the mesial edge of the freshly applied lingual shelf. A 0.5mm frame extending more than halfway through the contact point was created and cured. The process was repeated on tooth 2.1 with the goal of recreating both lingual and proximal walls of the restoration, leaving only the facial volume to be replaced.
Fig. 2. Pre-crimped Mylar matrix repeated on the DIBP aspect of tooth 2.1 to close the available space. CLEARFIL MAJESTY™ ES-2 Universal UL is used here.
Block-out of the composite extensions against the natural tooth structure was achieved by opacification using an opaque composite resin (WD, CLEARFIL MAJESTY™ ES-2 Premium, Kuraray Noritake Dental Inc.) layered in both horizontal and vertical increments. It is noted that the restorative join line must be completely obscured at the end of layering the dentin volume, otherwise the case will have almost certain esthetic failure. The internal dentin anatomy and its inherent variation was created to mirror that of the 2.1, which had minimal compromise of its incisal window with details intact. A super translucent composite resin (Clear, CLEARFIL MAJESTY™ ES-2 Premium, Kuraray Noritake Dental Inc.) was placed between the lobes of the dentin layers and cured. A 9:1 ratio of white: orange tint was mixed and placed on the incisal edge and proximoincisal corners to recreate the halo effect. A pure white tint was placed in gentle dentin mamelon-connecting spider legs up to the incisal edge to impart the realism. This was layered in a manner consistent with the appearance of the 2.1.
Fig. 3. Both horizontal and vertical dentin composite increments are demonstrated mimicking the contralateral tooth.
Fig. 4 & 5. Final immediate post-operative result after finishing and polishing.
DISCUSSION
The esthetic merit of this case is foundationally supported by composite resin technology on multiple levels. The color and physical stability over time needs to be proven in order for the clinician to have faith in its prognostication. Specifically, the material needs to have an excellent and well-matched refractive index, and one that is unaffected by both water and thermocycling stressors.
The palatal shelf was fabricated using a new-generation super nano-filled universal composite system that boasts a strong chameleon effect. If it is our intention to fool the eye, to obscure, then this first layer works well to start the blockout process of the darkness of the mouth behind the fracture line of the restored tooth. Following this, the chroma and value of the tooth are corrected using the dentin, simultaneous to its continued opacification of the fracture line and intraoral darkness. Both dentin and enamel layers are applied histoanatomically, that is, in a manner respecting the various thickness zones observed in nature.
Ultimately, esthetic success in direct composite resin is not dictated on the first day post-operatively. Factors are in play, from dehydration to occlusal wrinkles that need to be ironed out and corrected. The win depends on what material is used, along with how that material was developed to what standards, and why shade accuracy is so important in a world of variety. In a dental world with myriad composite options, we are looking for precision. Precision in technology leads to efficiency and physicoesthetic maintenance in clinical results. This ultimately results in a boost to clinician-patient confidence and an optimal prognosis.
Dentist:
CLARENCE TAM
*VITA is a trademark of VITA Zahnfabrik, Bad Sackingen, Germany
References
1. Elamin HO, Abubakr NH, Ibrahim YE. Identifying the tooth shade in group of patients using Vita Easyshade. Eur J Dent. 2015 Apr-Jun;9(2):213-217. doi: 10.4103/1305-7456.156828. PMID: 26038652; PMCID: PMC4439848.
2. Floriani F, Brandfon BA, Sawczuk NJ, Lopes GC, Rocha MG, Oliveira D. Color difference between the vita classical shade guide and composite veneers using the dual-layer technique. J Clin Exp Dent. 2022 Aug 1;14(8):e615-e620. doi: 10.4317/jced.59759. PMID: 36046166; PMCID: PMC9422970.
3. Gurrea J, Gurrea M, Bruguera A, Sampaio CS, Janal M, Bonfante E, Coelho PG, Hirata R. Evaluation of Dental Shade Guide Variability Using Cross-Polarized Photography. Int J Periodontics Restorative Dent. 2016 Sep-Oct;36(5):e76-81. doi: 10.11607/prd.2700. PMID: 27560681.
4. Almasabi W, Tichy A, Abdou A, Hosaka K, Nakajima M, Tagami J. Effect of water storage and thermocycling on light transmission properties, translucency and refractive index of nanofilled flowable composites. Dent Mater J. 2021 May 29;40(3):599-605. doi: 10.4012/dmj.2020-154. Epub 2020 Dec 24. PMID: 33361663.
5. Arai Y, Kurokawa H, Takamizawa T, et al.. Evaluation of structural coloration of experimental flowable resin composites. J Esthet Restor Dent. 2020;e12674.
6. Ota M, Ando S, Endo H, et al.. Influence of refractive index on optical parameters of experimental resin composites. Acta Odontol Scand. 2012;70(5):362–367.
7. Suliman S, Sulaiman TA, Olafsson VG, Delgado AJ, Donovan TE, Heymann HO. Effect of time on tooth dehydration and rehydration. J Esthet Restor Dent. 2019 Mar;31(2):118-123. doi: 10.1111/jerd.12461. Epub 2019 Feb 23. PMID: 30801926.
8. Meng Z, Yao XS, Yao H, Liang Y, Liu T, Li Y, Wang G, Lan S. Measurement of the refractive index of human teeth by optical coherence tomography. J Biomed Opt. 2009 May-Jun;14(3):034010. doi: 10.1117/1.3130322. PMID: 19566303.
9. Tekçe N, Demirci M, Sancak EI, Güder G, Tuncer S, Baydemir C. Clinical Performance of Direct Posterior Composite Restorations in Patients with Amelogenesis Imperfecta. Oper Dent. 2022 Nov 1;47(6):620-629. doi: 10.2341/21-106-C. PMID: 36281978.