Interview with Mathias Fernandez Y Lombardi
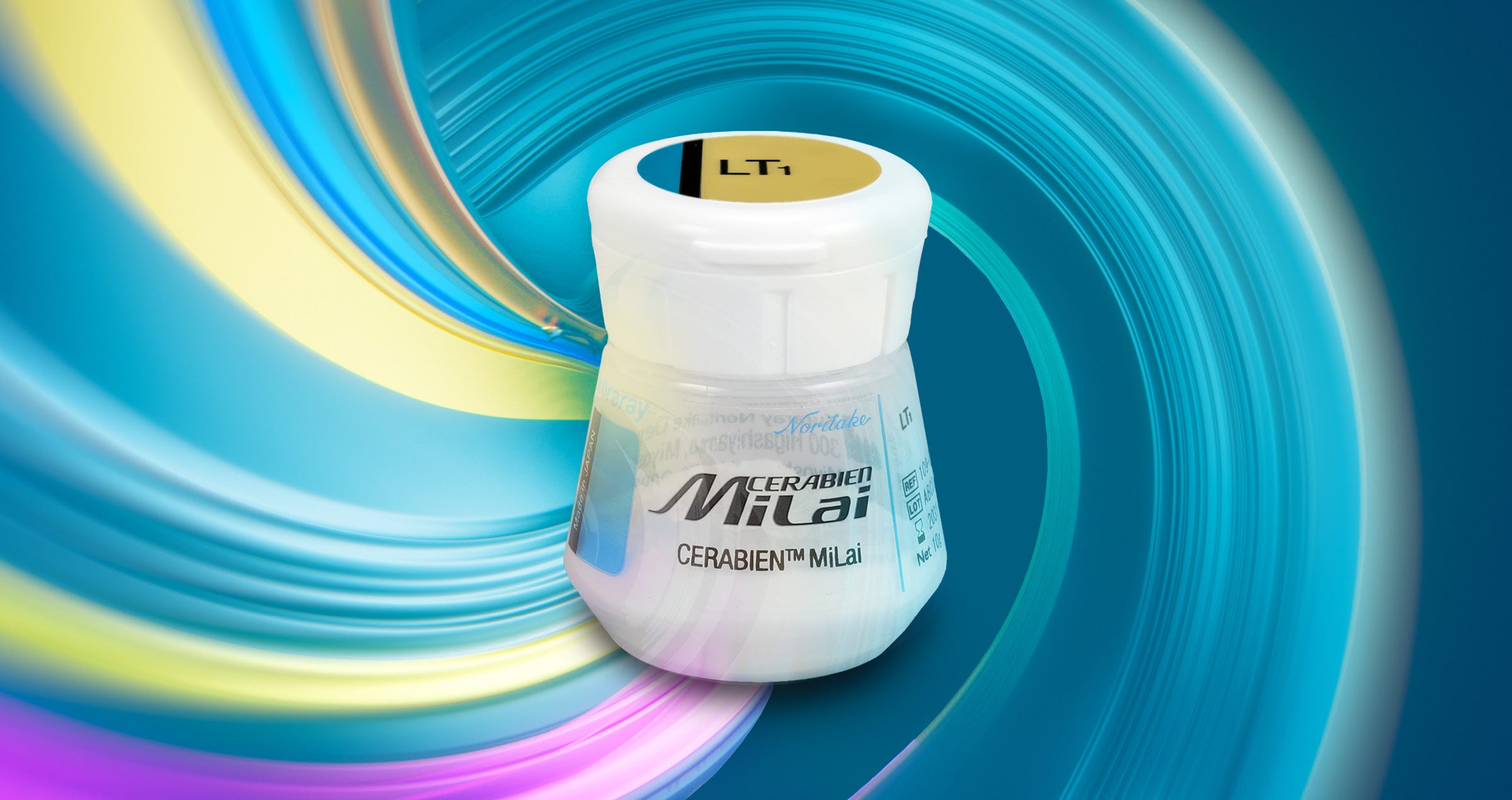
INTRODUCING CERABIEN™ MiLai LOW-FUSING PORCELAINS AND INTERNAL STAINS
Highly aesthetic lithium disilicate or zirconia-based framework materials combined with a micro-layer of porcelain are becoming the new standard for producing lifelike all-ceramic restorations. For those wondering why it’s worth adopting the new technique, how to start, how to improve and which materials to use, we had a conversation with a true expert in all things ceramic: Mathias Fernandez Y Lombardi, Head of Technical Marketing – Europe at Kuraray Europe GmbH.
Mathias Fernandez Y Lombardi, do you believe in micro-layering as a technique that is capable of streamlining procedures in the dental laboratory while fulfilling high aesthetic demands?
Yes, I truly believe that micro-layering is the next step in the evolution of indirect restorative techniques and materials. This evolution is driven by improvements in the area of framework materials, which are becoming more and more tooth-like in their appearance. We have moved from metal to opaque, high-strength zirconia and – more recently - high-translucency multi-layered zirconia and lithium disilicate, which no longer require thick porcelain layers to achieve lifelike outcomes. In this context, it’s only natural that a new technique has emerged.
Kuraray Noritake Dental Inc. is well-known as a pioneer in multi-layered zirconia technology and veneering porcelains. Are there any products particularly suitable or specifically developed for micro-layering?
We offer a series of high-translucency, multi-layered zirconia perfectly suited for micro-layering on the one hand and an aligned portfolio of internal stains and porcelains specifically developed for micro-layering on the other. The zirconia portfolio includes three different blank types with a multi-layered colour structure (KATANA™ Zirconia UTML, STML and HTML Plus), one variant with flexural strength, translucency and colour gradation (KATANA™ Zirconia YML), but also the timeless classic HT for the frameworks should be mentioned. While the first three offer a uniform strength and are chosen based on the indication, KATANA™ Zirconia YML with its multi-layered strength is a universal material suitable for an extremely wide range of applications.
The set of internal stains and porcelains specifically designed for the micro-layering technique that we just introduced is CERABIEN™ MiLai. With this addition to the CERABIEN™ family, we offer a perfect complement to the KATANA™ Zirconia Multi-Layered series, and with it, a revolutionary workflow that significantly deviates from traditional methods, enabling us to deliver greater efficiency, cost savings, and more flexibility. However, CERABIEN™ MiLai is not only compatible with KATANA™ Zirconia, but also with aesthetic zirconia from other manufacturers and reinforced silicate ceramics such as lithium disilicate with a CTE value within 9.5-11.0×10-6/K (50 °C – 500 °C).
Fig. 1. Overview of CERABIEN™ MiLai Low-Fusing Porcelains.
Fig. 2. Overview of CERABIEN™ MiLai Internal Stains.
Why should a dental technician start using the micro-layering technique and invest in a new set of porcelains for this purpose?
The reasons to start micro-layering are obvious: depending on the design, micro-layering can eliminate or minimize the chipping risk. Moreover, the technique is highly efficient, as the number of layers and bakes is drastically reduced. This results in a reduced thickness of the restoration facilitating minimally invasive preparations and a less complex layering procedure that even beginners are able to learn and implement very quickly. A new set of porcelains specifically developed for micro-layering like CERABIEN™ MiLai can further support the feasibility of the technique and the quality of the outcomes achieved even by beginners. Due to the shortage of skilled workers in dental laboratories, this aspect is becoming increasingly important.
How does CERABIEN™ MiLai support users in achieving aesthetic, high-quality outcomes right from the start?
With traditional porcelain systems, it can be challenging to create all the desired individual shade effects in a layer of only 0.03 mm to 0.6 mm thickness. With CERABIEN™ MiLai, this isn’t the case as the system is specifically designed for this purpose. The saturation and translucency of the porcelains are matched to the framework materials and adjusted to the volume of the porcelain layer. The compact line-up makes it quite easy to select and combine the right shades for satisfying results right from the start. More experienced users can mix the different components for additional effects, so that there are no limits to their creativity.
Images courtesy of MDT Daniele Rondoni.
Fig. 3. Virtually unlimited design options: crown with a full micro cut-back, crown with a vestibular cut-back and monolithic restoration.
Furthermore, the versatility of CERABIEN™ MiLai is a key feature that results in great outcomes. The system can be used on lithium disilicate and zirconia, a monolithic surface, a vestibular cut-back or a full micro cut-back. With this broad application spectrum, dental technicians are likely to use CERABIEN™ MiLai daily, which allows them to develop a true understanding of the components and to establish work routines very quickly. As a consequence, the outcomes become predictable and controllable. This is further supported by consistent handling and optical properties – all the result of a single core technology.
Please tell us more about this technology.
The core technology used in CERABIEN™ MiLai is synthetic feldspathic ceramic technology. Originally developed for Super Porcelain EX-3 and adjusted to the specific needs of CERABIEN™ ZR in the first step and CERABIEN™ MiLai more recently, this technology is responsible for consistent properties. This is because the formulation never needs to be aligned due to changing natural components. However, I believe that the greatest benefit of using feldspathic porcelain lies in the elimination of shadow effects. Everyone familiar with layering natural feldspathic porcelains on ceramics will know the typical greyish shadows appearing in restorations after several firing cycles. They originate from inhomogeneities in the material caused by micro-movements during firing. Showing no movements in this phase, synthetic felspathic porcelains from Kuraray Noritake Dental Inc. are the first and only porcelains preventing this effect. Finally, the further developed version of the technology allowed us to realize a low firing temperature of just 740 °C while maintaining the desired coefficient of thermal expansion. This is essential for the material’s compatibility with lithium disilicate.
Are there any other benefits arising from the low firing temperature?
The low firing temperature definitely offers an economic benefit, as the process consumes less energy and takes less time compared to high-temperature firing cycles. Moreover, the wear of the furnace is reduced. Finally, the low temperature is of interest for users of CERABIEN™ ZR in specific indications: Some ceramists like to combine the systems especially in cases with artificial gingiva. They create the porcelain work on the teeth with CERABIEN™ ZR first and then individualize the gingival area with CERABIEN™ MiLai. Due to the low firing temperature, the form, colour and surface of the previously applied veneering porcelain will remain stable.
Image courtesy of MDT Ioulianos Moustakis.
Fig. 4. Application of CERABIEN™ MiLai Tissue Porcelains on a complex restoration with the teeth already finalized.
Image courtesy of MDT Ioulianos Moustakis.
Fig. 5. Application of CERABIEN™ MiLai Internal Stains on a zirconia bridge.
Do you have any application technique recommendations for CERABIEN™ MiLai?
The best aesthetic outcomes are obtained by using the internal stain technique. By applying the stains first, it is possible to create natural depth effects despite the minimal thickness of the porcelain layer. The stains are easy to use and the outcomes are impressive. The micro-layer of porcelain applied on top acts like a window imitating the enamel, which contributes to a tooth-like appearance. Due to the compact line-up and easily manageable effects, this technique is even suitable for beginners.
Is the procedure different depending on the base material (lithium disilicate versus zirconia)?
Most of the steps are identical. However, surface conditioning may be different depending on the material used (as described in the material manufacturer’s instructions for use). Moreover, Value Liner 1 or Value Liner 2 is typically used on lithium disilicate for wash baking, whereas Translucent or Luster are recommended for this step on zirconia. When space is limited, internal stains may be applied directly. All following steps – the optional but highly recommended application of internal stains, the building-up of Translucent or Luster and baking, morphological corrections, the glaze bake and finishing – are identical.
What are the options for glazing?
CERABIEN™ MiLai porcelains offer a self-glaze effect obtained by fine-polishing (with PEARL Surface C) followed by glaze baking. This leads to a natural gloss, while maintaining the anatomical details. Alternatively, CERABIEN™ ZR FC Paste Stain Glaze or Clear Glaze can be applied and fixed by baking. These liquid ceramics allow users to add some structural details, while the surface appears glossier. However, the procedure is more time-consuming due to the additional application step.
Do you have any recommendations regarding the indication-specific selection of the framework or base material?
Traditionally, lithium disilicate has been the material of choice for aesthetic single anterior restorations, while zirconia was predominantly used for multi-unit restorations and restorations in the posterior area. With the availability of KATANA™ Zirconia STML / UTML and CERABIEN™ MiLai, zirconia is becoming increasingly attractive for the production of minimally invasive veneers, crowns and the like. A thin-walled restoration made of KATANA™ Zirconia, speed-sintered in just a few minutes and combined with a thin layer of CERABIEN™ MiLai, results in an incredibly strong restoration with several aspects that lithium disilicate simply cannot match. The preparation technique for zirconia is much more favourable for dentists - for example marginal adaptation and biocompatibility, especially regarding gingival healing, are superior. Aesthetically, there is no risk of a greyish effect when using zirconia with CERABIEN™ MiLai, while lithium disilicate needs to be treated with Value Liner to prevent this. Additionally, the ease of cementation with PANAVIA™ SA Cement Universal further enhances the quality of the restoration in the fastest possible timeframe, allowing for quick and flexible responses to dentists’ needs.
You mentioned speed sintering as a factor contributing to a streamlined workflow. Studies have shown, however, that this step might weaken the mechanical and aesthetic properties of zirconia. Do you recommend speed sintering despite this fact?
Indeed, speed sintering does affect the translucency and flexural strength of some zirconia variants. This is probably the reason why dental technicians have been reluctant to change their established practices of sintering overnight – despite the availability of high-speed furnaces. However, KATANA™ Zirconia is an exception: Due to our unique powder formulation, we are able to offer zirconia with a composition that is completely independent from other brands of dental zirconia. With this, we are able to fundamentally change the traditional workflow of an end-user and offer more flexibility, speed and efficiency, resulting in less energy consumption, stress and costs. In a study conducted at the Division of Biomaterials at the University of Alabama at Birmingham1, three different high-translucency zirconia materials including KATANA™ Zirconia Block (KATANA™ Zirconia STML) were sintered according to a traditional and a high-speed sintering schedule. Prior to sintering and afterwards, the three-point bending strength, translucency and grain structure were analysed. The material from Kuraray Noritake Dental Inc. was the only zirconia with properties that remained unaffected after speed sintering. Internal testing confirmed this finding for all variants of the KATANA™ Zirconia Multi-Layered series. As a result, we do recommend speed sintering of our materials, delivering true economic and time advantages.
With highly potent materials for micro-layering now available, do you think that full ceramic layering is going to be a thing of the past?
I am convinced that in the near future the great majority of dental restorations will be produced using aesthetic framework materials and simplified micro-layering techniques. However, full porcelain layering is here to last. There will always be a demand for a few highly-skilled ceramists serving the needs of individuals with the highest aesthetic demands. It is like tailor-made versus off-the-peg suits: the tailor-made ones are the best you can buy, but most people wear off-the-peg ones, which are perfectly adequate in virtually every environment.
Thank you very much!
Reference
1. Lawson NC, Maharishi A. Strength and translucency of zirconia after high-speed sintering. J Esthet Restor Dent. 2020 Mar;32(2):219-225. doi: 10.1111/jerd.12524. Epub 2019 Sep 13. PMID: 31515932.
Mathias Fernandez Y Lombardi
EU Scientific Manager
Dental Ceramics & CAD/CAM Materials
Kuraray Europe GmbH
2013
Successful completion of an apprenticeship as a dental technician at Seuthe dental laboratory in Plettenberg, Germany
2018
Successful completion of dental technology studies at the University of Osnabrück, Germany. Graduation as an engineer in dental technology
Since March 2018
Employee of Kuraray Europe GmbH