By Dr. PhD. Jusuf Lukarcanin
Is it possible to fulfil high aesthetic demands by restoring anterior teeth with composite resin? It is – provided that several important factors are respected. One of these factors is the faithful reproduction of the natural tooth morphology, which has a decisive impact on aesthetics and function. Moreover, success is determined by the selection of the right shades of high-quality composite resin and their purposeful combination using proper layering techniques.
Introduction
The aesthetic appearance of direct anterior restorations is affected by proper shade selection on the one hand and the creation of a natural shape and texture on the other1. Hence, the dental practitioner’s own artistic skills play a decisive role. According to Fahl, information about the tooth morphology and function, and the optical properties of the tooth should be taken into consideration when the most suitable restorative material and shade are selected2.
These minimally invasive composite restorations are no longer a temporary solution for the anterior region. Instead, they are regarded as an adequate alternative to indirect restorations, as they are both durable and able to closely imitate the natural tooth structure34.
Clinical case example 1
This 45-year-old female patient presented with a diastema and a disproportion in the size and shape of her maxillary central incisors (Fig. 1). In the first step, a detailed case history was taken and an intra-oral examination was carried out. Subsequently, the initial situation was recorded by taking intra-oral photographs, which would allow for a computer-aided morphological evaluation and treatment planning (Fig. 2).
Fig. 1: Pre-operative image.
Fig. 2: Digital mock-up.
The patient’s second visit started with a professional tooth cleaning procedure followed by isolation of the maxillary anterior teeth. Afterwards, the tooth shade was determined and appropriate composite shades were selected. In this case, the shades A2E, Amber Translucent and A3D of CLEARFIL™ Majesty ES-2 Premium (Kuraray Noritake Dental, Japan) appeared to be most suitable. In addition, a mock-up was created using mock-up resin in order to produce a silicone key.
Opting for a minimally invasive procedure, no mechanical tooth preparation using drills was performed after removal of the mock-up. Instead, the enamel was merely etched with 35% phosphoric acid gel (K-Etchant, Kuraray Noritake Dental) to increase the surface roughness. After rinsing and drying, the adhesive agent (CLEARFIL™ Universal Bond, Kuraray Noritake Dental) was applied to the etched surfaces. Composite layering started with the build-up of palatal shells with the aid of the silicone key. Following light-curing of the shells, a small amount of composite in the dentin shade A3D was applied to the proximal surfaces using a thin spatula and a brush. The aim was to reduce light transmission in the area of the dentin core. The restoration was completed with a combination of the composite shades A2E (enamel) and Amber Translucent, which were applied using a modeling brush.
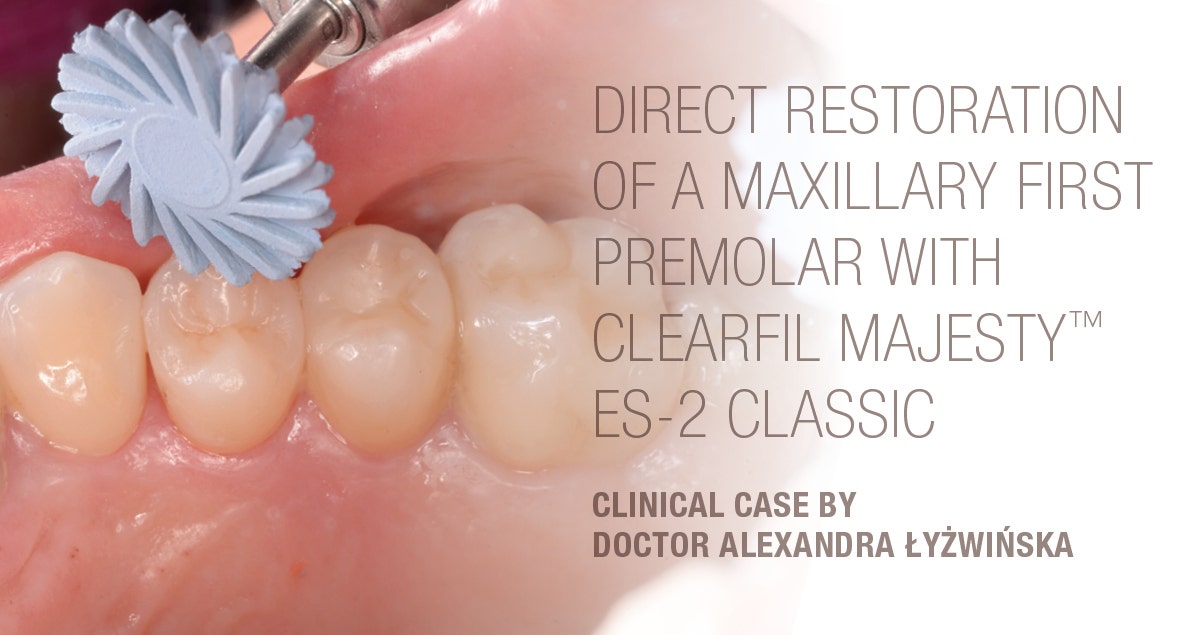
Finishing and polishing was accomplished using flexible rubber polishing discs containing diamond particles (CLEARFIL™ Twist DIA, Kuraray Noritake Dental) with a low-speed handpiece. No additional finishing and contouring was necessary due to the use of a brush during layering, which ensured the creation of a natural shape and surface texture. Figure 3 shows the outcome of the restoration procedure.
Fig. 3: Treatment outcome immediately after polishing.
Oral hygiene training was provided and follow-up examinations were performed after three, six and twelve months (Fig. 4). Healthy hard and soft tissue conditions were observed during these visits.
Fig. 4: Clinical situation at the one-year recall.
Clinical case example 2
This 30-year-old female patient had a diastema, irregularly shaped anterior teeth and showed signs of abrasive tooth wear (Fig. 5). Following a detailed anamnesis and intra-oral examination, the tooth shade was determined and the composite CLEARFIL™ Majesty ES-2 Premium selected in the monochromatic shade Universal A1.
Fig. 5: Pre-operative clinical situation.
Following the isolation of the working field, 35% phosphoric acid etchant (K-Etchant) was applied to the enamel of all teeth between the maxillary right canine and the maxillary left first molar. The surfaces were then treated with a universal bonding agent (CLEARFIL™ Universal Bond) as recommended by the manufacturer. Modeling was carried out with a thin spatula and a modeling brush for composite. Neither a silicone key nor any wetting or modeling resin were used in the procedure. For polishing, the flexible polishing discs CLEARFIL™ Twist DIA were used at low rotational speed. Thanks to the use of the modeling brush, no additional finishing with diamond-coated instruments was necessary. Figures 6 and 7 show the final restoration at baseline and one week after completion of the treatment.
Fig. 6: Treatment outcome at the day of the restorative procedure.
Fig. 7: Clinical situation after one week.
This patient also received oral hygiene training and presented for recalls three, six and twelve months after the treatment. The patient maintained an exemplary oral hygiene behaviour, so that it came as no surprise that the soft tissues were healthy and the restorations were in a perfect condition after one year (Fig. 8).
Fig. 8: Clinical situation one year after the restorative treatment.
Discussion
Nowadays, direct composite restorations are becoming increasingly popular. Especially for young patients and all those who do not want to sacrifice large amounts of healthy tooth structure, the technique is an ideal treatment option5. In many cases, aesthetic outcomes are possible without mechanical tooth preparation, but a selective etching procedure only6.
The clinical lifetime of these restorations depends on many factors. Important prerequisites for high-quality outcomes include the selection of a suitable composite material with the required surface hardness, appropriate finishing and polishing, a good oral hygiene behaviour, and proper maintenance measures during periodical follow-up visits. As a matter of course, the manual skills of the dental practitioner and the use of selected materials according to the manufacturer’s instructions for use also have a direct impact on the long-term success of the restorations789. A user’s inability to meet one of these requirements and failure to carry out all working steps correctly may have a direct impact on the quality of the restoration.
Conclusion
Composite resin is a popular material class for the production of aesthetic anterior restorations die to their straightforward use and rapid application, good repair options and high aesthetic potential when used properly . The two case examples illustrate that a treatment with composite resin is often the best treatment option when a non-invasive procedure completed within a single visit is desired.
About the author
Dr. Jusuf Lukarcanin is a Certified Dental Technician (DCT) and a Doctor of Dental Science (DDS). He studied dentistry at the Ege University Dental Faculty in Izmir, Turkey, where he obtained a Master‘s degree in 2011. In 2017, he received a Ph.D. degree from the Department of Restorative Dentistry of the same university. Between 2012 and 2019, Dr. Lukarcanin was the head doctor and general manager at a private clinic in Izmir. Between 2019 and 2020, he worked at Tinaztepe GALEN Hospital as a Restorative Dentistry specialist, between 2020-2022 he worked at MEDICANA International Hospital Izmir as a Restorative Dentistry specialist. Currently he is an owner of a private clinic for aesthetics and cosmetics in Izmir.
References
1. Heymann HO (1987) The artistry of conservative esthetic dentistry Journal of the American Dental Association 115(Supplement)14-23.
2. Fahl N Jr (2012) Single-shaded direct anterior composite restorations: A simplified technique for enhanced results Compendium of Continuing Education in Dentistry 33(2) 150-154.
3. Barrantes, J. C. R., Araujo Jr, E., & Baratieri, L. N. (2014). Clinical Evaluation of Direct Composite Resin Restorations in Fractured Anterior Teeth. Odovtos-International Journal of Dental Sciences, (16), 47-61.
4. Vargas M (2011) Clinical techniques: Monocromatic vs. polycromatic layering: How to select the appropriate technique ADA Professional Product Review 6(4) 16-17.
5. Ferracane, J. L. (2011). Resin composite—state of the art. Dental materials, 27(1), 29-38.
6. Norling, N. A. (2010). Combining “prep-less” and conservatively prepared veneers to correct enamel defects and asymmetry. Journal of Cosmetic Dentistry, 2010.
7. Ölmez, A., & Kisbet, S. (2012). Kompozit rezin restorasyonlarda bitirme ve polisaj işlemlerindeki yeni gelişmeler. Acta Odontologica Turcica, 30(2), 115-22.
8. Senawongse, P., & Pongprueksa, P. (2007). Surface roughness of nanofill and nanohybrid resin composites after polishing and brushing. Journal of Esthetic and Restorative Dentistry, 19(5), 265-273.
9. Giacomelli, L., Derchi, G., Frustaci, A., Bruno, O., Covani, U., Barone, A., Chiappelli, F. (2010). Surface roughness of commercial composites after different polishing protocols: an analysis with atomic force microscopy. The open dentistry journal, 4, 191.
10. Hickel, R., Heidemann, D., Staehle, H. J., Minnig, P., & Wilson, N. H. F. (2004). Direct composite restorations. Clin Oral Invest, 8, 43-44.
11. Korkut, B., Yanıkoğlu, F., & Günday, M. (2013). Direct composite laminate veneers: three case reports. Journal of dental research, dental clinics, dental prospects, 7(2), 105.