Unlock the power of zirconia: perfect for adhesive cementation, the ideal material for a wide range of indications, and essential in minimal invasive dentistry. Time to trust zirconia bonding!
This article demystifies zirconia bonding, providing clear, practical steps to ensure long-term functionality and patient satisfaction, all based on scientific research. Master the three adhesion pillars: mechanical retention, chemical activation, and wetting capacity. Discover how to successfully prepare zirconia surfaces, avoid pitfalls like misapplying silica coating and silane, and choose proven bonding systems for optimal results. Optimise retention even with minimal tooth preparation and achieve reliable zirconia restorations. Say goodbye to doubts and hello to successful zirconia bonding!
Factors influencing retention
Loss of retention due to de-cementation or debonding is a common cause of dental prostheses' failure. First, let’s have a look at how to cope with the three main factors significantly influencing retention: tooth preparation, restoration pre-treatment, and cement type/bonding.
Tooth preparation
The abutment tooth's height, angle, and surface texture must be considered to achieve sufficient retention and resistance from the preparation. The retention form counteracts tensile stresses, whereas the resistance counteracts shear stresses 4. With the proper preparation, a restoration resists dislodgement and subsequent loss.
Full coverage restorations
To achieve sufficient retention and resistance for full-coverage crowns, the tooth abutment should be at least 4 mm high, and the convergence angle should range from 6 to 12 degrees with a maximum of 15 degrees 1, 5-8.
Source; Conventional cementation or adhesive luting - A guideline, Dr. A. Elsayed, Prof. Dr Florian Beuer
Adhering to the tooth preparation guidelines is crucial for full-coverage restorations (e.g., crowns, and FDPs). These practical guidelines are designed to achieve the required retention and resistance to make conventional luting possible. However, optimal retention and resistance are, in reality, hard to achieve. An unwanted amount of sound tooth substance often should be removed to achieve a highly retentive preparation. Moreover, several studies2,3 show that, in daily practice, the preparation angle often exceeds 15 degrees.
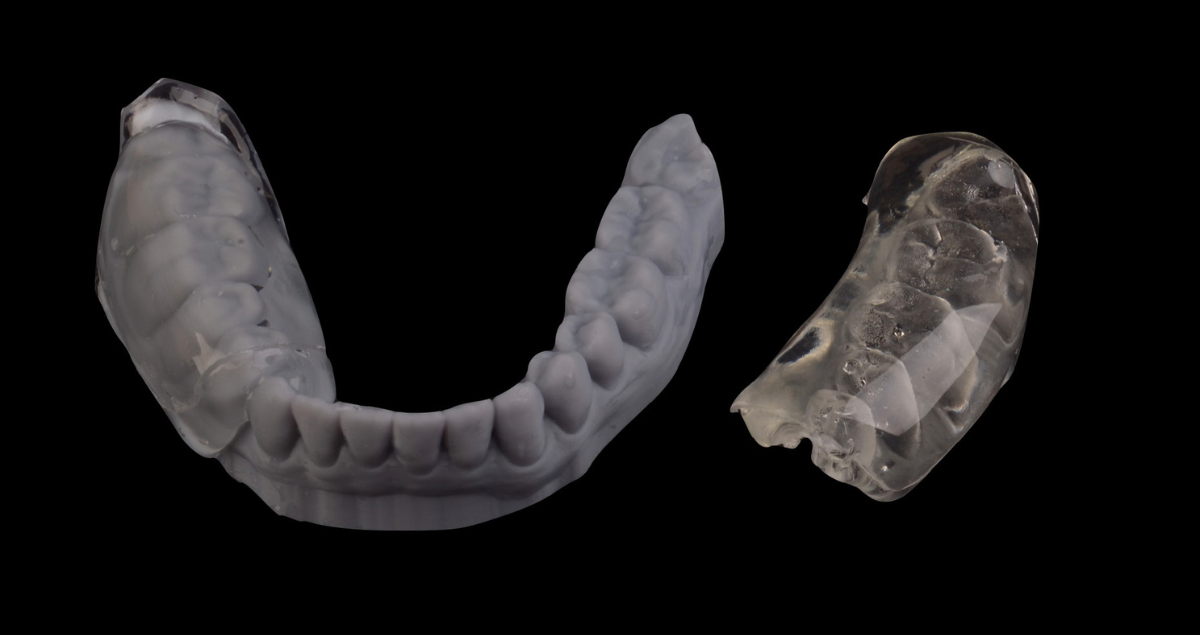
Minimal-invasive restorations
Minimal-invasive restorations, such as single retainer FDPs, veneers, table-tops and inlay-retained FDPs, are based on a non- or low-retentive preparation form. In this case, retention shifts from (macro-)mechanical to micro-mechanical and chemical, necessitating the use of adhesive techniques 9-11. Even though the preparations for minimal-invasive restorations largely lack mechanical retention, the long-term success of these types of restorations is well-documented when using a suitable resin cement (e.g. PANAVIA™, Kuraray Noritake Dental, Japan), including a proper pre-treatment and bonding procedure 10, 11.
In high-retentive situations, conventional luting is acceptable for full-coverage restorations*. In all other cases, choosing a resin cement is a better solution. With proper tooth preparation (e.g., shaping, (self-)etching, abrasion) and the right adhesive resin cement system, a non-retentive preparation form provides a reliable basis using mainly chemical retention and micro-mechanical retention instead of macro-mechanical retention.
*Please review the articles available regarding the debate over whether to use a conventional cementation procedure, adhesive cementing, or selective adhesive luting
Restoration pre-treatment
Zirconia is densely sintered and does not contain a glass phase. Therefore, it cannot be etched with hydrofluoric acid to create a micro-retentive etching pattern. In addition, silanes cannot effectively promote zirconia bonding. Several studies have shown that air abrasion with 50-µm alumina at a reduced pressure of 0.5 bar (0.05 MPa; 7 psi) will create a sufficient micro-retentive pattern12 and greatly enhances the wetting capacity.
In addition to air abrasion, chemical coupling agents such as bifunctional phosphate resin monomers are used on air-abraded zirconia. Bonding with phosphate monomer-containing adhesive resin systems gives very reliable results27,28. The use of phosphate monomer-based resin cement systems (e.g., Panavia [Kuraray Noritake Dental, Tokyo, Japan]) and/or phosphate monomer primers, such as CLEARFIL CERAMIC Primer Plus (Kuraray Noritake Dental, Tokyo, Japan) on freshly air-abraded zirconia, offer the most reliable bonding methods today 13,27,28. We therefor consider MDP-based composite resin cements the material choice for our bonding procedure. However, it must be stressed that contamination of the air-abraded zirconia with saliva, phosphoric acid or other contaminants will limit the formation of chemical bonds and, therefore, must be avoided.
Avoiding contamination
For optimal moisture control, absolute isolation of the working field is crucial. Minimising the risk of contamination, avoiding exposure to oral fluids. Before restoration placement, a thorough cleaning of the abutment tooth is essential. Following trial placement, a meticulous recleaning step is recommended to remove any potential introduced contamination. KATANA Cleaner (Kuraray Noritake Dental, Tokyo, Japan) is an ideal choice due to its unique properties. Its slightly acidic pH of 4.5 allows for effective cleaning intraoral and extraoral adhesion surfaces. Additionally, the incorporation of MDP monomer technology makes it highly efficient. The MDP salt in this product effectively bonds with contaminants, breaks them down and results in easy removal by water rinsing.
Cement type/bonding
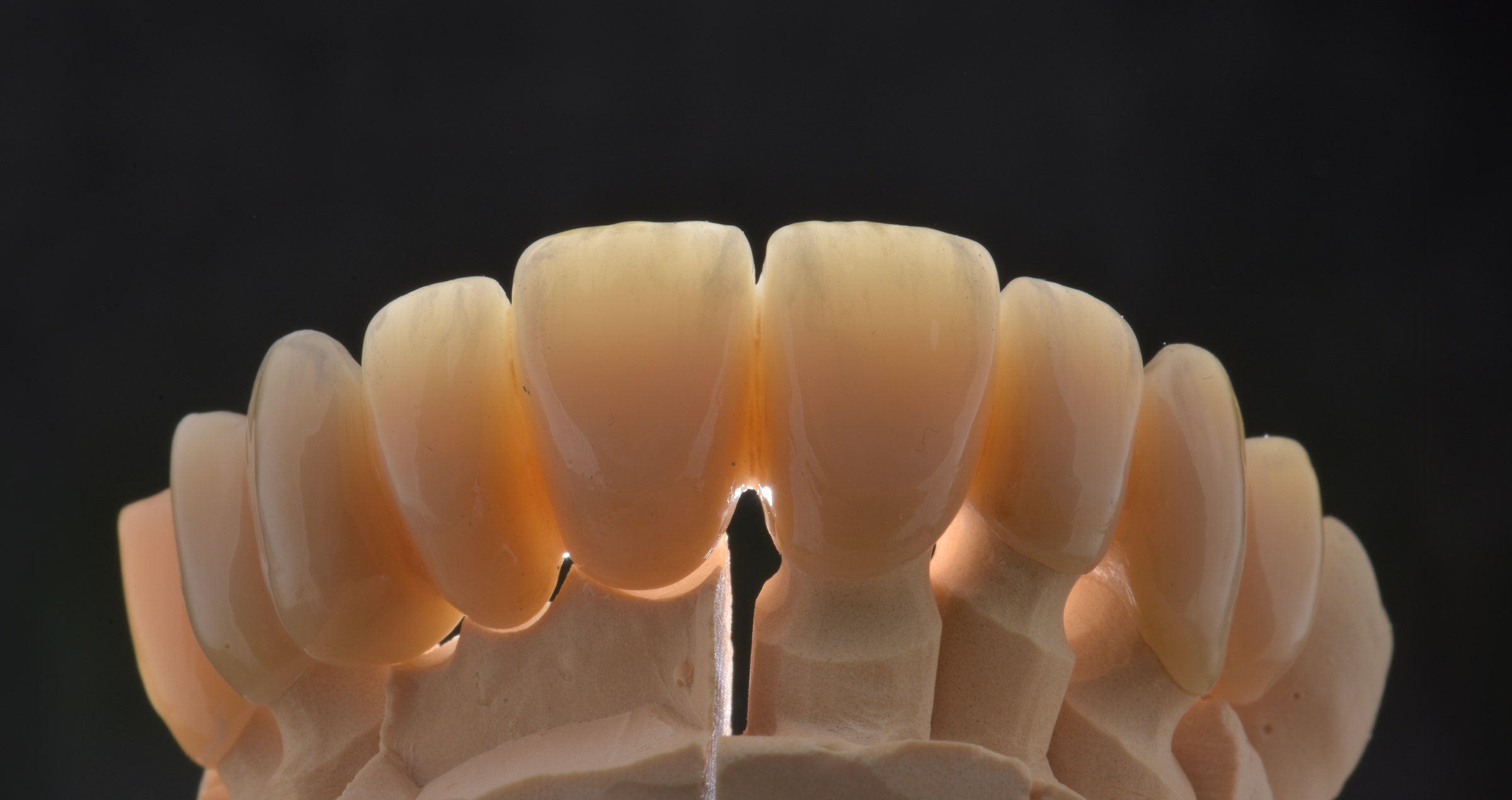
After pre-treatment of surfaces to optimise the , it is important to understand that the properties of highly translucent zirconia differ highly from those of earlier generation zirconia. Early-generation zirconium oxides, including 3 mol% yttrium oxide (3Y-TZP), are high in strength and low in translucency. With the increase in yttria, creating 4-5 mol% yttria, or higher, zirconium oxides, the number of cubic crystals increases, resulting in higher translucency but leading to a reduction in strength. Therefore, attention must be paid to zirconia type, material thickness, restoration type, and application area. These factors may influence the choice of cement based on the adhesive properties demanded for lasting restorations and high aesthetic outcomes.
PANAVIA™ V5
For a resin cement system to deliver a strong bond, it is not always enough to have it contain an appropriate adhesive monomer. It is necessary for that adhesive monomer to be polymerised effectively under different circumstances. The PANAVIA™ V5 system contains an innovative “ternary catalytic system” consisting of a highly stable peroxide, a non-amine reducing agent* and a highly active polymerisation accelerator. Since this catalytic system is amine-free, the hardened cement has unsurpassed colour stability. In addition, the highly active polymerisation accelerator, one of the components in PANAVIA™ V5 Tooth Primer, is not only an excellent reducer that promotes polymerisation effectively, but it is also capable of coexisting with the (in this product) acidic MDP. This makes it possible to create a single-bottle self-etching primer. This accelerator is also responsible for the so-called touch-cure reaction when it comes into contact with the paste. Resulting in the sealing of the dentin interface and, at the same time, allowing the paste to set even in situations where light curing is limited.
*PANAVIA™ V5 Tooth Primer applied and left for 20 seconds, followed by air drying.
The second primer in the PANAVIA V5 system is CLEARFIL™ CERAMIC PRIMER PLUS, which incorporates Kuraray Noritake Dental’s original MDP and a silane. This product is used to prime zirconia but is also an excellent choice for priming silica-based ceramics, composites, and metals.
CLEARFIL™ CERAMIC PRIMER PLUS, which contains the original MDP, applied and dried.
The PANAVIA™ V5 full adhesive resin cement system consists of all three above-mentioned components, always used in the same way, independent of the material, for a straightforward procedure to ensure reliable bonding. The PANAVIATM V5 systems offer try-in pastes to visualise the final results before final cementing and confirm the appropriate shade of the resin cement to be used.
PANAVIA™ VENEER LC
Offering a flexible workflow and high bondability of thin, translucent restorations like veneers but also inlays and onlays, PANAVIA™ Veneer LC was designed. It is a light-curing resin cement system allowing a long working time of 200 seconds under ambient light*. This allows multiple veneers to be placed simultaneously without racing against the setting. The final light-curing can be started anytime after positioning the provisions. The PANAVIA™ Veneer LC cementing system includes PANAVIA™ Tooth Primer and CLEARFIL CERAMIC PRIMER Plus as primers to chemically interact with the adhesive surfaces.
PANAVIA™ Veneer LC Paste applied and the laminate veneer seated. In this case six veneers were simultaneously placed during one session.
Unpolymerized excess paste removed with a brush. PANAVIA™ Veneer LC Paste is a light-cured type rein cement, designed to provide sufficient working time.
This photo shows the results after the final light curing. Since the excess cement was easily removed, there were almost no cement residues.
PANAVIA™ SA CEMENT Universal
Still, clinicians seek efficiency and effectiveness in everyday practice by using a straightforward but durable resin cement solution. PANAVIA™ SA Cement Universal is developed to offer this ease-of-use property without losing focus on bonding properties. PANAVIA™ SA Cement Universal is developed with the original MDP monomer in the hydrophilic paste compartment, allowing for chemical reactiveness with zirconia and tooth structure. The other compartment contains the hydrophobic paste, to which a unique silane coupling agent, LCSi monomer, is added, which allows the cement to deliver a strong and durable chemical bond to silica-based materials like porcelain, lithium disilicate and composite resin*. Furthermore, PANAVIA™ SA Cement Universal is less moisture sensitive than full adhesive resin cement systems. This also makes it the ideal cement in situations where rubberdam isolation is difficult.
*The product is available in both auto mix and hand mix options.
*Old PFM bridge (shown here) removed, and existing preparations modified to accommodate a 3-unit KATANA™ Zirconia bridge. The upper right canine was prepared to receive a single-unit KATANA™ crown.
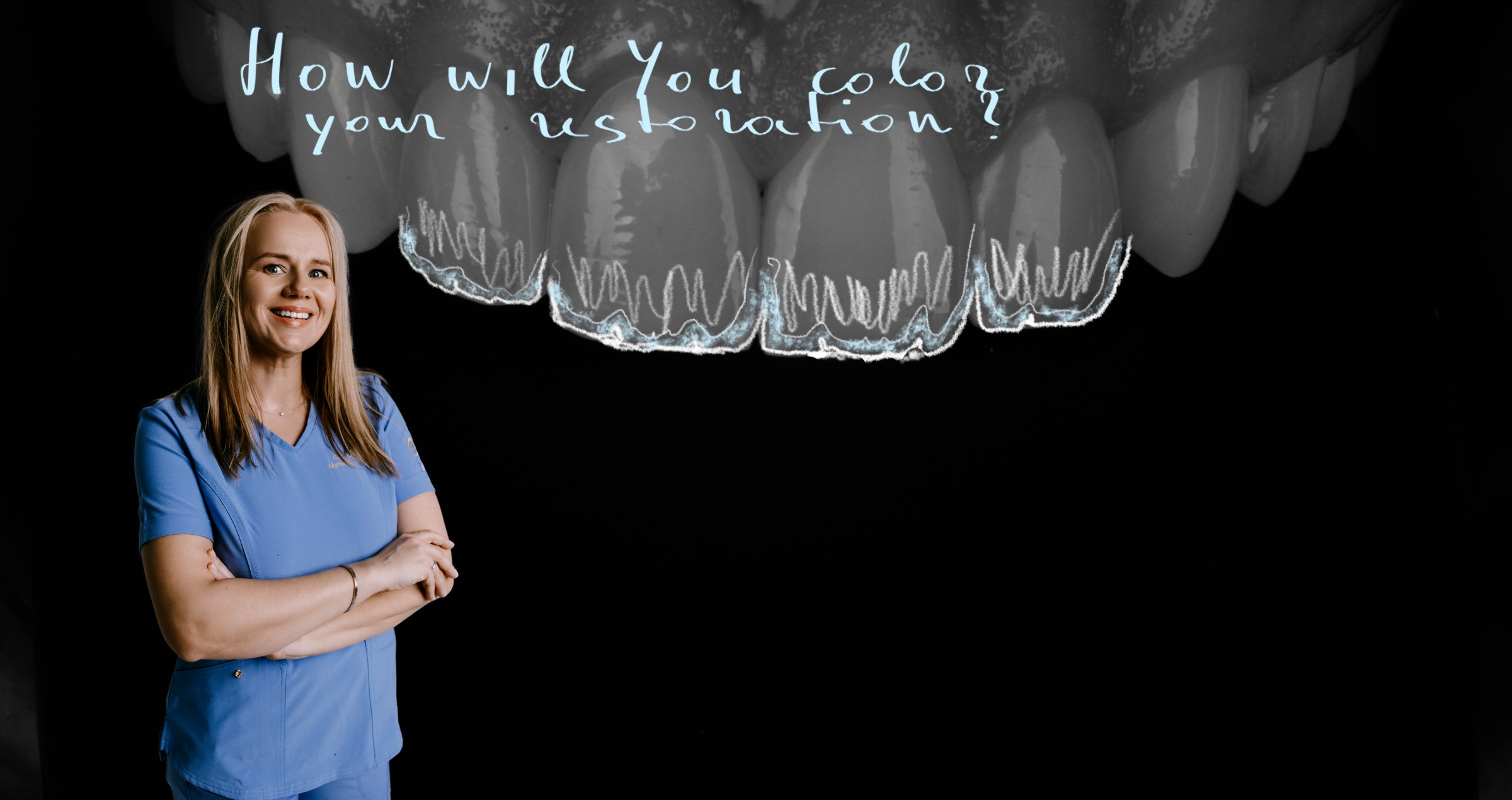
Before
After. Seating & Final Smile. PANAVIA™ SA Cement Universal and CLEARFIL™ Universal Bond Quick were used for cementation and bonding. “I love the ease of use and clean-up with PANAVIA™ SA Cement Universal, and its MDP monomer creates a strong chemical bond to the tooth structure and zirconia. CLEARFIL™ Universal Bond Quick has a quick technique without reducing bond strengths, releases fluoride and has a low film thickness. I simply rub CLEARFIL™ Universal Bond Quick into the tooth for a few seconds and air dry. There is no need to light-cure, since it cures very well with PANAVIA™ SA Cement Universal. The patient was very happy with the results. She loved that she no longer saw metal margins, and her smile was much more uniform and lifelike.” Dr. Kristine Aadland
*Images are a part of a case by Dr. Kristine Aadland; 3-Unit anterior maxillary
Bonding to zirconia in three steps
Over the last century, the popularity of highly translucent zirconia has skyrocketed due to its excellent properties and wide range of anterior and posterior clinical applications. Because zirconium oxide prostheses are, if processed correctly, antagonist-friendly and easy (and relatively inexpensive) to fabricate, the material keeps gaining popularity in dentistry.
Several steps need to be taken into account for reliable and durable bonding. Years of research on achieving high and long-term bond strength to zirconia have concluded into three practical steps, summarised as the APC concept13 as a reliable procedure guideline.
APC-Step A
Zirconia should be air-particle abraded (APC-Step A) with alumina or silica-coated alumina particles; the sandblasting or micro-etching procedure. Air abrasion with a chairside micro-etcher using aluminium oxide particles (size: up to 50 μm) at a low pressure of 0,5 bar (0.05 – 0.25 MPa) is sufficient.14,18,25-27
APC-Step P
The subsequent step includes applying a special ceramic primer (APC-Step P), which typically contains specially designed adhesive phosphate monomers, onto the zirconia adhesive surfaces.29,30 The MDP monomer has been shown to be particularly effective at bonding to metal oxides like zirconium oxide.
APC-Step C
Dual- or self-cure resin cement systems should be used to reach an adequate C=C conversion rate underneath the zirconia restoration since the lack of translucency in zirconia reduces light transmission.13 However, in cases where high-translucent zirconia (HTZr02) is used, the zirconia transmits light so that the shade of composite or resin cement might influence the final appearance of such restorations. It is, thereforebased on the individual situation and shade of the abutment tooth.
The APC zirconia-bonding concept is not limited to intra-oral situations and can also be applied in the laboratory for implant reconstructions that include cemented zirconia components.
Conclusion
Rapid developments in high-quality translucent zirconia have made the utility and reliability of adhesive cementing systems even more crucial. This applies to fully opaque restorations but also minimally invasive and ultra-translucent restorations of low thickness. In all cases, the longevity of the bonding and, thus, the provision directly affects patient satisfaction. By taking into account the three primary parameters we have discussed in this article and following the predictable APC protocol, you will successfully realise durable bonded zirconia restorations from now on.
References
- Ladha K, Verma M. Conventional and contemporary luting cements: an overview. J Indian Prosthodont Soc. 2010;10(2):79-88.
- Nam, Y., Eo, M.Y. & Kim, S.M. Development of a dental handpiece angle correction device. BioMed Eng OnLine17, 173 (2018). https://doi.org/10.1186/s12938-018-0606-1
- Florian BEUER, Daniel EDELHOFF, Wolfgang GERNET, Michael NAUMANN, Effect of preparation angles on the precision of zirconia crown copings fabricated by CAD/CAM system, Dental Materials Journal, 2008, Volume 27, Issue 6, Pages 814-820
- Muruppel AM, Thomas J, Saratchandran S, Nair D, Gladstone S, Rajeev MM. Assessment of Retention and Resistance Form of Tooth Preparations for All Ceramic Restorations using Digital Imaging Technique. J Contemp Dent Pract. 2018;19(2):143-9.
- Edelhoff D, Özcan M. To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: cementation. Clin Oral Implants Res. 2007;18 Suppl 3:193-204.
- Güth JF, Stawarczyk B, Edelhoff D, Liebermann A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int. 2019;50(7):512-20.
- Smith CT, Gary JJ, Conkin JE, Franks HL. Effective taper criterion for the full veneer crown preparation in preclinical prosthodontics. J Prosthodont. 1999;8(3):196-200.
- Uy JN, Neo JC, Chan SH. The effect of tooth and foundation restoration heights on the load fatigue performance of cast crowns. J Prosthet Dent. 2010;104(5):318-24.
- Blatz MB, Vonderheide M, Conejo J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J Dent Res. 2018;97(2):132-9.
- Chaar MS, Kern M. Five-year clinical outcome of posterior zirconia ceramic inlay-retained FDPs with a modified design. J Dent. 2015;43(12):1411-5.
- Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51-5.
- Kern M, Dr Med Habil, M. BONDING TO ZIRCONIA. Jerd_40. 3DOI 10.1111/j.1708-8240.2011.00403.x VOLUME 2 3 , NUMBER 2 , 2011
- Blatz MB, Alvarez M, Sawyer K, Brindis M. How to Bond Zirconia: The APC Concept. Compend Contin Educ Dent. 2016 Oct;37(9):611-617; quiz 618. PMID: 27700128.
- Blatz M.B., Oppes S., Chiche G., et al. Influence of cementation technique on fracture strength and leakage of alumina all-ceramic crowns after cycling loading. Quintessence Int. 2008; 39(1): 23-32
- Burke F.J., Fleming G.J., Nathanson D., Marquis P.M. Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent. 2002;4(1)): 7-22
- Blatz M.B. Sadan A., Maltezos C., et al. In vitro durability of the resin bond to feldspathic ceramics. AM J Dent 2004;17 (3):169-172
- Blatz M.B., Bergler M. Clinical applications of a new self-adhesive resin cement for zirconium-oxide ceramic crowns. Compend Contin Educ Dent. 2012;33(10):776-781
- Maggio M., Bergler M., Kerrigan D., Blatz M.D. Treatment of maxillary lateral incisor agenesis with zirconia-based all-ceramic resin bonded fixed partial dentures: a case report. Amer J esthet Dent. 2012;2(4):226-237
- Ozer F., Blatz M.B., Self-etch and etch-and0rinse adhesive systems in clinical dentistry. Compend Contin Edus Dent. 2013;24 (1):12-20
- Kern M., Thomson V.P., Bonding to glass infiltrated alumina ceramic: adhesive methods and their durability. J Prosthet Dent. 1995;73 (3):240-249
- Kern M., Wegner S.M., Bonding to zirconia ceramics: adhesion methods and their durability. Dent Mater. 1998;14(1):64-71
- Wegner S.M., Kern M. Long-term resin bond strength to zirconia ceramic. J Adhes Dent. 2000;2 (2):139-147
- Blatz M.B., Sadan A., Martin J., Lang B. In vitro evaluation of shear bond strength of resin to densely-sintered high-purity zirconium-oxide ceramics after long-term sorage and thermos cycling. J Posthet Dent. 2004;9(4):356-362
- Blatz M.B., Chiche G., Holst S., Sadan A. Influence of surface treatment and simulated aging on bond strength of luting agents to zirconia. Quintessence Int. 2007;38 (9):745-753
- Quaas A.C., Yang B., Kern M., Panavia F 2.0 bonding to contaminated zirconia ceramic after different cleaning procedures. Dent Mater. 2007;23(4):506-512
- Song J.Y., Park S.w., Lee K., et al. Fracture strength and microstructire of Y-TZP zirconia after different surface treatments. J Prosthet Dent. 2013;110(4):274-280
- Koizumi H., Nakayama D., Komine F., et al. Bonding of resin-based luting cements to zirconia with and without the use of ceramic priming agent. J adhes Dent. 2012;14(4):385-392
- Nakayama D., Koizumi H., Komine F., et al. Adhesive bonding of zirconia with single -liquid acidic primers and a tri-n0butylborane initiated acrylic resin. J Adhes Dent. 2010;12(4):305-310
- Alnassar T., Ozer F., Chiche G., Blatz M.B. Effect of different ceramic primers on shear bond strength of resin-modified glass ionomer cement to zirconia. J Adhes Sci Technol. 2016;DOI:10.1080/01694243.1184404
- Blatz M.B. Long-term clinical success of all-ceramic posterior restorations. Quintessence Int. 2002;33(6):415-426
- Mante F.K., Ozer F., Walter R., et al. The current state of adhesive dentistry: a guide for clinical practice. Compend Contin Educ Dent. 2013;34:Spec 9:2-8
- Ozcan M., Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17(1):7-26
- Inokoshi M., De Munck J., Minakuchi S., Van Meerbeek B. Meta-analysis of bonding effectivenss to zirconia ceramics. J Dent Res. 2014;93(4):329-334