BUSTING MYTHS AROUND HIGH-STRENGTH CERAMICS IN DENTISTRY
Crowns, bridges, partial restorations: When it comes to replacing or restoring an individual’s teeth with fixed dental prostheses, the choice is often between the high-strength ceramics - lithium disilicate and zirconia. Originally, the higher aesthetic potential of silicate ceramics made them particularly suitable for single tooth restorations, while the high-strength option zirconia was predominantly used for bridges and frameworks. Due to continuous improvements in the development of dental ceramics and adhesive technology, things have changed. Many of the original limitations and restrictions are no longer valid, and new opportunities arise for users in the dental setting.
In the following, we will address certain persisting myths about the use of zirconia and lithium disilicate in dentistry. In this context, you will receive an update on what is possible with the materials today and guidance on how and when to use them.
1. ZIRCONIA IS AESTHETICALLY INFERIOR TO LITHIUM DISILICATE
The original zirconia used in dentistry was whitish-opaque. Therefore, it was used as a framework material only. To create aesthetic restorations, it was necessary to apply a relatively thick layer of veneering porcelain. More recent generations of zirconia, however, include variants with a particularly high translucency and a multi-layered colour structure. These variants allow for less complex finishing techniques such as micro-layering or external staining. KATANA™ Zirconia UTML (Kuraray Noritake Dental Inc.), for example, is one of the most translucent zirconia materials on the dental market. Depending on the test method used, it offers a similar or only somewhat lower translucency compared to lithium disilicate (IPS e.max CAD LT, Ivoclar Vivadent)1-4. The desired natural result is achieved as light reaches – and reflects – the underlying tooth structure. Consequently, true-to-life restorations can be produced in an efficient, highly automated workflow.
CONCLUSION
Depending on the variant of zirconia and lithium disilicate used, both materials offer similar aesthetic properties, while even the highest-translucency zirconia is stronger than the highest-strength lithium disilicate available. Material selection may therefore be based on other criteria such as preparation depth for example.
2. ZIRCONIA-BASED RESTORATIONS ARE WEAKER THAN LITHIUM DISILICATE-BASED ONES DUE TO THE NEED OF A PORCELAIN LAYER ON TOP OF ZIRCONIA
This assumption is true for the first generations of dental zirconia. For modern zirconia materials with a high translucency and multi-layered colour structure, however, the situation is different. They are suitable for the production of monolithic restorations or restorations with a minimal (vestibular) cutback and a micro-layer of porcelain. With occlusal contact areas made of plain (polished or glazed) zirconia, these restorations are stronger than monolithic lithium disilicate restorations, while the chipping risk is minimized. In fact, even the weakest zirconia offers a significantly higher flexural strength than lithium disilicate (IPS e.max CAD LT, Ivoclar Vivadent)2,3. Thanks to the high edge stability of zirconia after milling, the restorations are also highly stable, a favourable property for long-term success.
CONCLUSION
The flexural strength of zirconia is generally higher than that of lithium disilicate (800 to 1,200 MPa for zirconia versus 360 to 460 MPa for lithium disilicate), and due to the improved aesthetic potential of the available materials, a full porcelain layer is no longer required. Hence, zirconia restorations are usually very strong and durable.
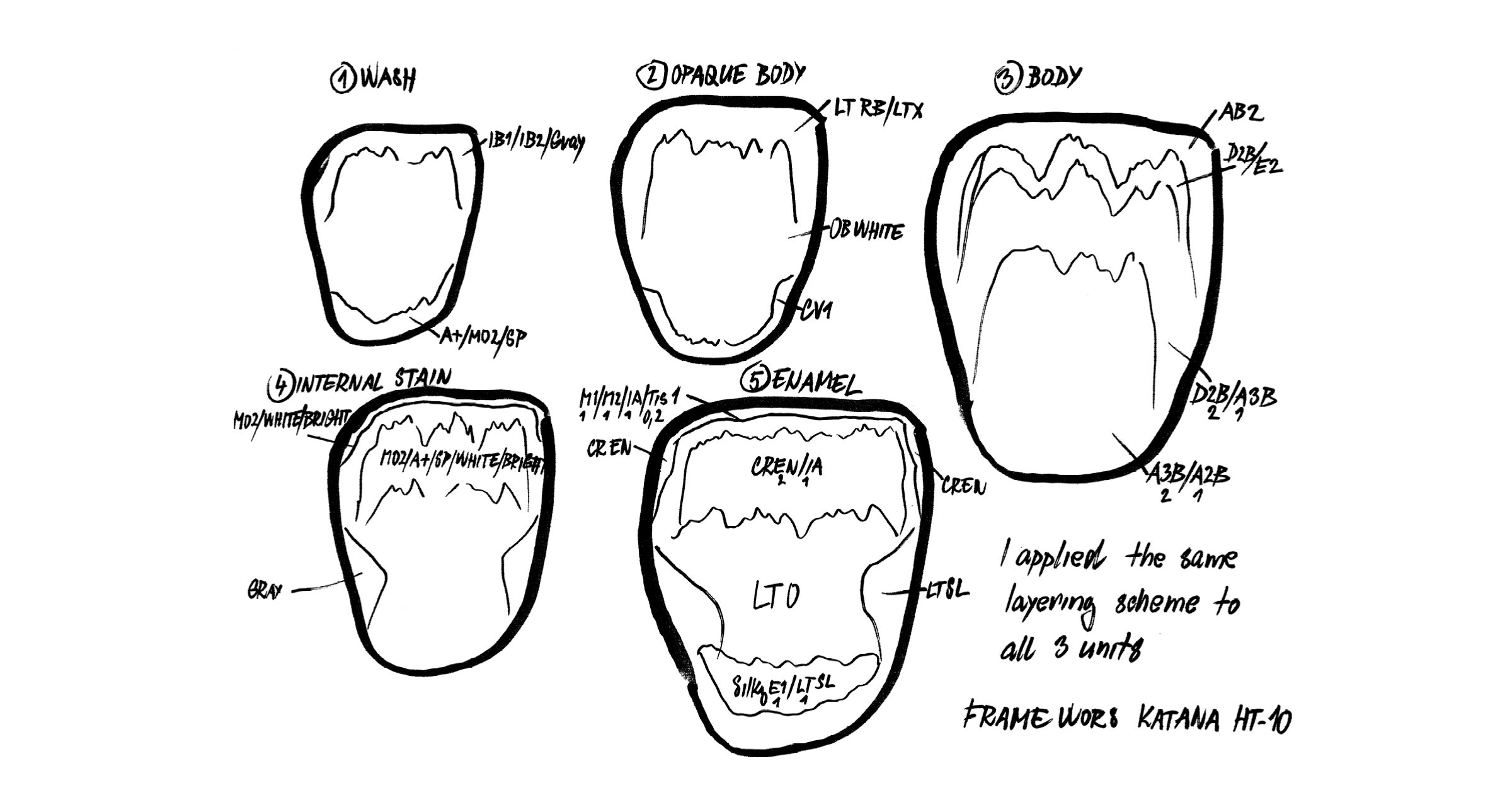
3. FINISHING OF ZIRCONIA RESTORATIONS IS MORE COMPLICATED THAN FINISHING OF LITHIUM DISILICATE RESTORATIONS
When using modern, aesthetic zirconia materials, finishing techniques are quite similar. The most popular technique for both, high-translucency zirconia and lithium disilicate, is micro-layering. Based on a full-contour restoration design and a subsequent cutback limited to the vestibular area, a micro-layer of porcelain (often a specific porcelain line-up developed for micro-layering) is applied. With CERABIEN™ MiLai from Kuraray Noritake Dental Inc., the standard procedure consists of internal staining, the application of luster porcelains and final glazing. Fewer layers and fewer bakes are required compared to full porcelain layering. However, aesthetic zirconia can also be used for the production of monolithic restorations, which are characterized with paste stains and glazed.
CONCLUSION
As a monolithic design or minimal cutback of restorations based on modern zirconia materials is an option, finishing of zirconia is just as easy as finishing of lithium disilicate restorations. The technique depends on the desired outcome.
4. ZIRCONIA-BASED RESTORATIONS ARE MORE INVASIVE THAN THOSE MADE OF LITHIUM DISILICATE
This myth is also based on the assumption that zirconia needs a thick porcelain layer on top to produce aesthetic results. Since this is not the case and great outcomes are possible with monolithic designs or micro-layering approaches, a minimally invasive preparation design is supported by the use of zirconia as a restorative material. Due to a comparatively high strength even of the high-translucency variants, the minimum wall thickness is quite low (e.g. 0.4 mm for veneers made of KATANA™ Zirconia UTML or STML and 0.5 mm for posterior crowns made of KATANA™ Zirconia HTML Plus)*. This allows for a defect-oriented tooth structure removal.
*In general, the minimum wall thickness depends on the product and the indication.
CONCLUSION
Depending on the type of zirconia and the finishing method, zirconia supports the production of minimally invasive restorations.
5. DUE TO THEIR HARDNESS, MONOLITHIC ZIRCONIA RESTORATIONS HARM THE OPPOSING DENTITION
When manufacturers of dental zirconia started promoting the monolithic use of zirconia, in-vitro studies were soon available to prove that it is not the hardness of the material, but the smoothness of the surface that determines how kind or harmful a dental restoration is to the opposing dentition5-8. According to those studies, well-polished zirconia surfaces maintained their smoothness and showed a superior self-wear and wear to the opposing tooth structure compared to other restorative materials including lithium dislilicate6-8. As glaze - unlike the polished surface - tended to wear off over time, it was stressed that a perfectly polished restoration surface is essential for a wear-friendly long-term behaviour. The in-vitro study results were also confirmed in vivo9,10. According to the latest umbrella review focusing on this topic, polished monolithic zirconia causes lower antagonist enamel wear than metal ceramics, feldspathic porcelains and lithium disilicate tested10.
CONCLUSION
Provided that the surface is smooth, monolithic zirconia restorations are kind to the opposing natural tooth structure. Over time, the opposing enamel wear may be expected to be on a similar level as natural enamel wear.
6. ADHESIVE LUTING OF ZIRCONIA-BASED RESTORATIONS IS IMPOSSIBLE
When oxide ceramics like zirconia are processed and pre-treated in the same way as silicate ceramics like lithium disilicate, the obtained bond strength is lower. Using the correct pre-treatment protocol, however, it is possible to establish a strong and durable chemical bond between the tooth structure and the zirconia. Otherwise, it would not be possible to place single-retainer resin-bonded bridges made of high-strength zirconia (3Y-TZP) successfully, for example. Their design is largely non-retentive, so that a strong bond is of paramount importance. It is established by air-abrading the bonding surface of the zirconia retainer wing with aluminium oxide (50 μm) at a low pressure (approx. 1 to 2.5 bar) after try-in11,12, followed by ultrasonic cleaning, the use of a restoration primer that contains 10-MDP13 and the application of a high-performance resin cement like PANAVIA™ V5 (Kuraray Noritake Dental Inc.)14. Using this protocol with a predecessor of the resin cement just mentioned, ten-year survival and success rates were above 90 percent15. The described protocol is in line with the APC concept recommended by Prof Dr. Markus Blatz, which includes (A) airborne-particle abrasion, (P) zirconia primer, and (C) adhesive composite resin application16.
CONCLUSION
Using an appropriate protocol including small particle air-abrasion after try-in and a high-performance adhesive resin cement system with MDP primers, a strong and long-lasting chemical bond to zirconia can be established.
7. ZIRCONIA IS UNSUITABLE FOR RUSH CASES DUE TO THE NEED OF SINTERING THE RESTORATIONS AFTER MILLING
By using zirconia variants that are suitable for speed sintering, smaller restorations can be produced within very short time. Single-unit restorations and small bridges (up to three units) made of materials of the KATANA™ Zirconia Multi-Layered Series, for example, may be speed-sintered within 54 minutes, provided that a suitable furnace is used. This leads to a considerable reduction of the production time and is a great option for rush cases. For a true chairside workflow and same-day dentistry, KATANA™ Zirconia Block is a great option. It offers the same optical and mechanical properties as KATANA™ Zirconia STML and can be sintered even faster – in just 18 minutes.
CONCLUSION
By using suitable zirconia materials and equipment, production times of zirconia restorations are no longer an issue when it comes to rush cases.
8. ALL HIGH-STRENGTH CERAMICS HAVE A SIMILARLY WIDE RANGE OF INDICATIONS
In fact, the range of indications varies with the flexural strength and fracture toughness of the materials. While the use of lithium disilicate is limited to the production of single-tooth restorations and small bridges, zirconia typically covers a wider range of indications, with the high-strength variants being even suited for long-span bridges. The most versatile variants of zirconia are those with flexural strength gradient – like KATANA™ Zirconia YML. This material offers a particularly high translucency in the enamel layer and a high strength in the body layers. Therefore, it is well suited for the production of single-tooth restorations and of highly complex structures such as long-span bridges – depending on where the restoration is positioned in the disc.
CONCLUSION
Zirconia offers a wider range of indications than lithium disilicate. By selecting one of those variants with a multi-layered structure offering flexural strength gradation, it is possible to cover virtually every indication, while other variants are better suited for specific needs (highest translucency option for aesthetically demanding cases, highest strength option for complex long-span designs).
ZIRCONIA A TRUE ALLROUNDER
Modern versions of dental zirconia are high-performance materials with well-balanced optical and mechanical properties typically suitable for a wide range of indications. As a zirconia user, you may choose to employ a single material with flexural strength gradation for virtually every situation or prefer to select different products depending on case-specific demands. You have the freedom to select the preferred finishing technique from traditional layering to just polishing and may opt for minimally invasive restoration designs. The latter is due to proven protocols establishing a long-lasting bond to zirconia. For everyone with particularly high quality demands, the KATANA™ Zirconia Multi-Layered series is worth a try. The raw material composition is unique, the powder is developed in-house in Japan and the blanks are produced in a perfectly aligned procedure delivering a homogeneous, densely pressed material for restorations with an accurate fit, high strength and superior edge stability.
REFERENCES
1. F. Beuer, J. Schweiger, ConsEuro 2015 London, Kuraray Satellite Symposium, May 14th 2015.
2. Kwon SJ, Lawson NC, McLaren EE, Nejat AH, Burgess JO. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J Prosthet Dent. 2018 Jul;120(1):132-137.
3. Reale Reyes A, Dennison JB, Powers JM, Sierraalta M, Yaman P. Translucency and flexural strength of translucent zirconia ceramics. J Prosthet Dent. 2023 Apr;129(4):644-649.
4. Harada K, Raigrodski AJ, Chung KH, Flinn BD, Dogan S, Mancl LA. A comparative evaluation of the translucency of zirconias and lithium disilicate for monolithic restorations. J Prosthet Dent. 2016 Aug;116(2):257-63.
5. Janyavula S, Lawson N, Cakir D, Beck P, Ramp LC, Burgess JO. The wear of polished and glazed zirconia against enamel. J Prosthet Dent. 2013 Jan;109(1):22-9.
6. Preis V, Weiser F, Handel G, Rosentritt M. Wear performance of monolithic dental ceramics with different surface treatments. Quintessence Int. 2013 May;44(5):393-405.
7. Lawson NC, Janyavula S, Syklawer S, McLaren EA, Burgess JO. Wear of enamel opposing zirconia and lithium disilicate after adjustment, polishing and glazing. J Dent. 2014 Dec;42(12):1586-91. doi: 10.1016/j.jdent.2014.09.008. Epub 2014 Sep 23. PMID: 25257823.
8. Sripetchdanond J, Leevailoj C. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: an in vitro study. J Prosthet Dent. 2014 Nov;112(5):1141-50.
9. Hartkamp O, Lohbauer U, Reich S. Antagonist wear by polished zirconia crowns. Int J Comput Dent. 2017;20(3):263-274.
10. Shah N, Nerkar H, Badwaik P, Ahuja B, Malu R, Bhanushali N. An evaluation of antagonist enamel wear opposing full-coverage zirconia crowns versus other ceramics full-coverage crowns and natural enamel - An umbrella review. J Indian Prosthodont Soc. 2024 Jul 1;24(3):217-224.
11. Kern M. Bonding to oxide ceramics—laboratory testing versus clinical outcome. Dent Mater. 2015 Jan;31(1):8-14.
12. Kern M, Beuer F, Frankenberger R, Kohal RJ, Kunzelmann KH, Mehl A, Pospiech P, Reis B. All-ceramics at a glance. An introduction to the indications, material selection, preparation and insertion techniques for all-ceramic restorations. Arbeitsgemeinschaft für Keramik in der Zahnheilkunde. 3rd English edition, January 2017.
13. Al-Bermani ASA, Quigley NP, Ha WN. Do zirconia single-retainer resin-bonded fixed dental prostheses present a viable treatment option for the replacement of missing anterior teeth? A systematic review and meta-analysis. J Prosthet Dent. 2021 Dec 7:S0022-3913(21)00588-6.
14. Bilir H, Yuzbasioglu E, Sayar G, Kilinc DD, Bag HGG, Özcan M. CAD/CAM single-retainer monolithic zirconia ceramic resin-bonded fixed partial dentures bonded with two different resin cements: Up to 40 months clinical results of a randomized-controlled pilot study. J Esthet Restor Dent. 2022 Oct;34(7):1122-1131.
15. Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017 Oct;65:51-55. doi: 10.1016/j.jdent.2017.07.003.
16. Blatz MB, Alvarez M, Sawyer K, Brindis M. How to Bond Zirconia: The APC Concept. Compend Contin Educ Dent. 2016 Oct;37(9):611-617; quiz 618.
DOWNLOAD
Would you like to continue reading as a PDF? Please leave your email address below.