Case by Andreas Chatzimpatzakis
Observe and copy: This is the key to nature-like dental restorations. There are many optical effects, colour transitions and morphological details in natural teeth that need to be taken in and understood – and replicating them is only possible for those who know exactly how their materials work. Once these skills are acquired, however, they enable a dental technician to produce their restorations as truly beautiful copies of nature. Even when restoring a single maxillary central incisor, the technique delivers outstanding – or inconspicuous - outcomes, as revealed by the following example.
Using high-quality, translucent and gradient-shaded zirconia frameworks and porcelains, the layering technique does not have to be highly complicated. Two bakes and a number of selected effect liquids, internal stains and porcelains are usually sufficient for outcomes that exceed expectations.
CASE EXAMPLE
In the present case, a young male patient had a quite opaque crown on his maxillary right central incisor that needed to be replaced. During shade selection in the dental laboratory (Fig. 1), it was observed that the cervical third of the adjacent central incisor is lighter than the rest. Its shade in other areas corresponded to B4 on the VITA classical A1-D4® Shade Guide. Hence, it was decided to use a somewhat lighter material for the framework and darken the restoration especially in the middle and incisal areas with internal stains.
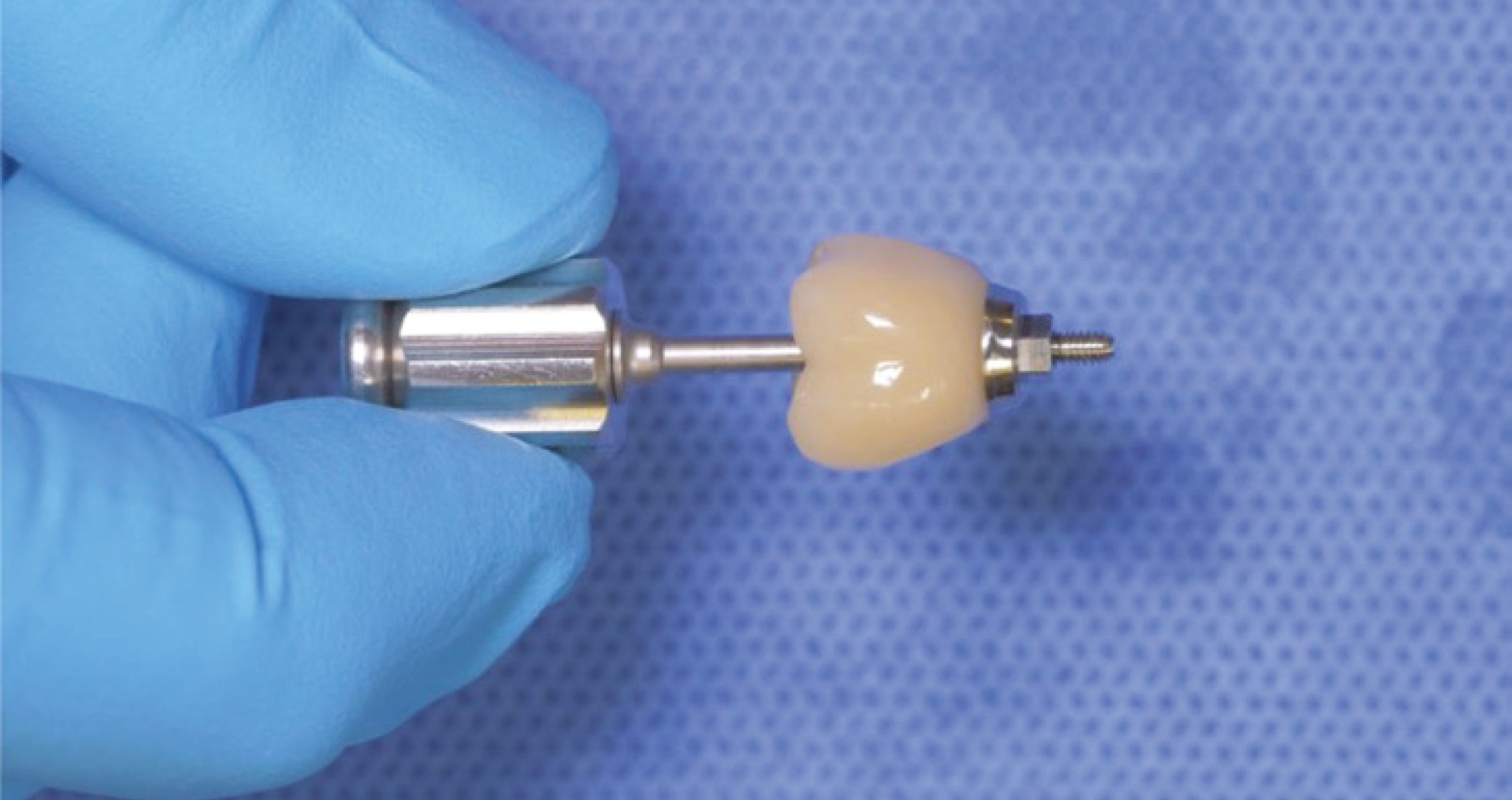
The concrete plan was to mill a coping made of KATANA™ Zirconia STML (Kuraray Noritake Dental Inc.) in the shade A3, characterize it with Esthetic Colorant (both Kuraray Noritake Dental Inc.) and sinter the piece (Figs 2 to 4). In the following layering procedure including just two bakes, a combination of internal stains and selected porcelains (CERABIEN™ ZR, Kuraray Noritake Dental Inc.) was applied as illustrated in Figures 5 to 12. Figures 13 to 17 display the result on the model, minor adjustments during try-in and the final treatment outcome.
Fig. 1. Shade selection. The cervical third of the adjacent central incisor is lighter than usual compared to the middle and incisal areas.
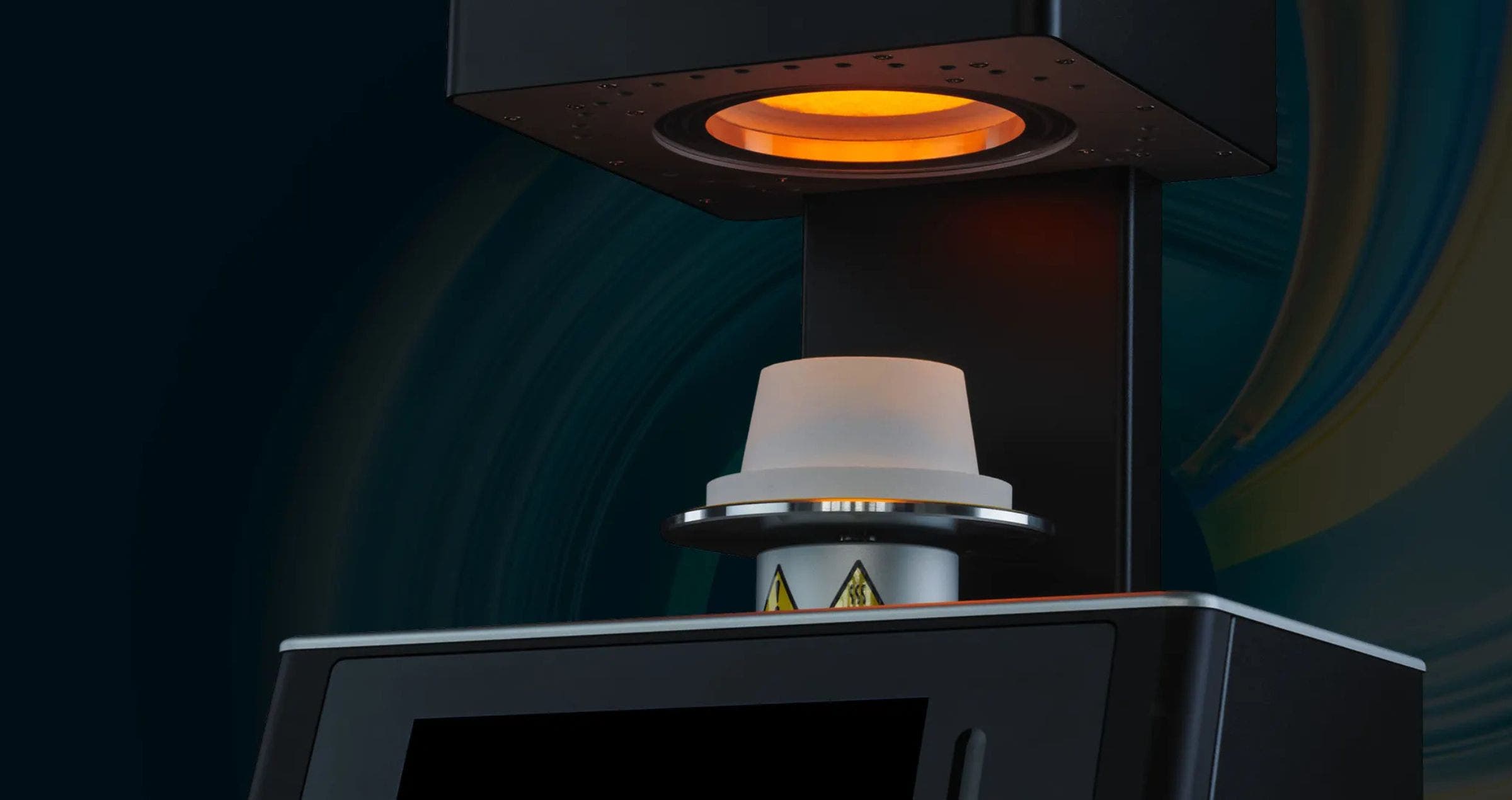
Fig. 2. Coping made of KATANA™ Zirconia STML in the shade A3.
Fig. 3. Intensification of some shade characteristics of the multi-layered blank using Esthetic Colorant in the shades Grey (middle) and Blue and Grey (incisal area).
Fig. 4. Coping after sintering.
Fig. 5. Colour map for internal staining, using CERABIEN™ ZR Internal Stains.
Fig. 6. Result of the use of Shade Base Stain Modifier Fluoro to increase the fluorescence and internal staining as planned.
Fig. 7. Application of Opacious Body OBA2, …
Fig. 8. … Translucent Tx …
Fig. 9.: … and Luster CCV-2.
Fig. 10. Crown after the first bake.
Fig. 11. Crown after the application of CERABIEN™ ZR Internal Stains: A+, Aqua Blue 2, White mixed with Cervical 2 (ratio: 30/70) for the cracks, and Cervical 2.
Fig. 12. Application of Luster LT1 to finalize the shape.
Fig. 13. Finished crown after the second bake on the model.
Fig. 14. Evaluation of the surface texture: Observing and copying the surface details is as important as the imitation of the shade characteristics.
Fig. 15. Minor texture adjustments during try-in.
Fig. 16. Final restoration in place after cementation with PANAVIA™ V5 (Kuraray Noritake Dental Inc.).
Fig. 17. Treatment outcome.
CONCLUSION
Mastering the art of observing natural teeth is the key to lifelike restorations. It allows a dental technician to develop a deep understanding of shade and morphology, which is – apart from knowing the selected materials very well – the only talent needed to reach a high level of excellence. Those who are observant and take in every detail with their eyes can be sure that their mind will understand and their hands will automatically follow.
Dental technician:
ANDREAS CHATZIMPATZAKIS
Andreas graduated from the Dental Technology Institute (TEI) of Athens in 1999. During his studies he followed a program at the Helsinki Polytechnic Department of Dental Technique, where he trained on implant superstructures and all ceramic prosthetic restorations. As of 2000, he is running the ACH Dental Laboratory in Athens, Greece, specialized on refractory veneers, zirconia and long span implant prosthesis. In 2017 Andreas visited Japan where he trained under the guidance of Hitoshi Aoshima, Naoto Yuasa and Kazunabu Yamanda and become International Trainer for Kuraray Noritake Dental Inc..