Case report by Vasilis Vasiliou
THE ART OF RESTORING SMILES: MASTERING THE CHALLENGE OF A SINGLE CENTRAL INCISOR
Restoring a single maxillary central incisor is possibly the biggest challenge a dental technician can face in everyday work. Especially when a patient is young, it is extremely important to restore her or his smile to its original beauty. Any restoration that is perceivable as such might have a negative impact on their self-confidence and quality of life even in the long term.
A STORY OF JOY AND DESPERATION
Take Ioanna, a 14-year-old girl who presented in her dental office in a state of desperation. In the hours before, she had been floating on cloud nine: Her favourite band performed in Cyprus for the first time and she had managed to buy tickets for herself and her best friend. Thrilled, they had arrived at the concert, the band started playing and the crowd danced to the music. It felt like this was going to be the best day of her life. At the time the band played its most popular song, people were delirious, jumping up and down in ecstasy. Between all the exuberant dancing and laughing, however, Ioanna suddenly was hit by a strong push. She fell, her face hitting something hard – a seat in front of her. Pain froze time and it took a few seconds before she understood what had happened: Tasting blood in her mouth, she explored her teeth with her tongue and realized that one of her central incisors had fractured.
AFFECTING THE QUALITY OF LIFE
This is one of the many touching stories we listen to every day. A fall during a concert, a push at somebody’s birthday party, a car accident: There are many incidences that can ruin a young, beautiful smile. By paying attention to the involved patients and their stories, one will come to realize how strongly some of them are affected by all this. They cover their mouths when they laugh or hold back their smiles.
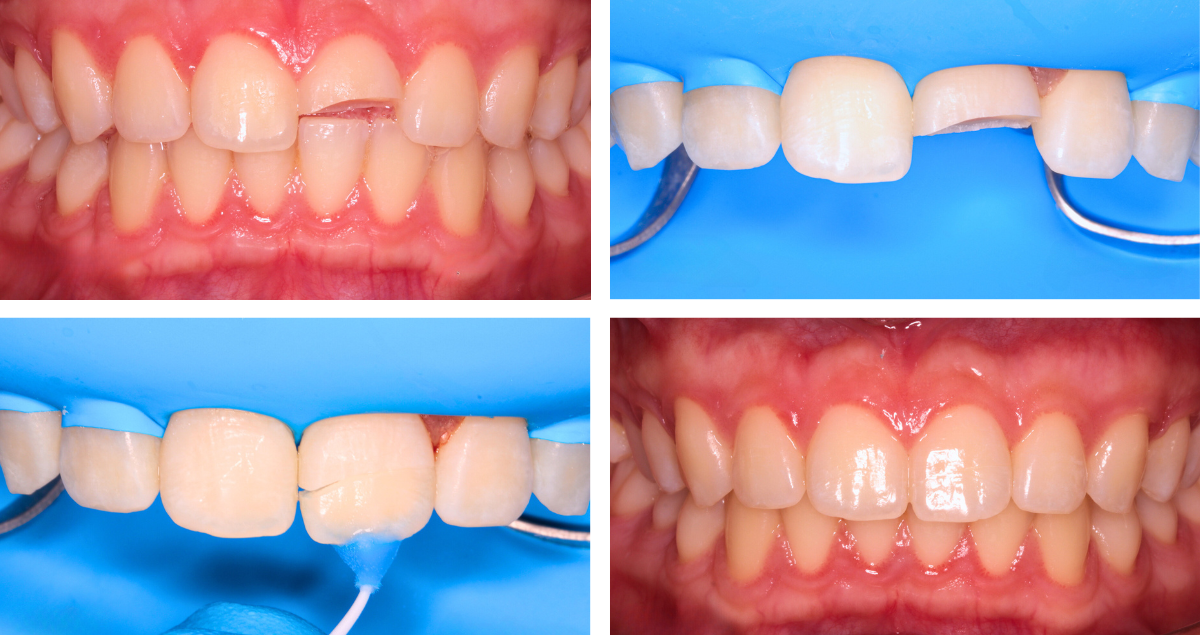
Any dental technician who is committed to restoring their lost smile in the best possible way is probably aware of the impact his or her work can have and the responsibility coming with it: A Beautiful result will restore not only their smile, but also their self-confidence, will let them start laughing happily, expressing themselves comfortably and simply enjoying social interaction again (Figs. 1 to 5). Compromised outcomes, on the other hand, might have the opposite effect. Being aware of this role should be every technician’s motivation to become better day by day. Evolve for these moments, when our work brings tears of joy to our patients.
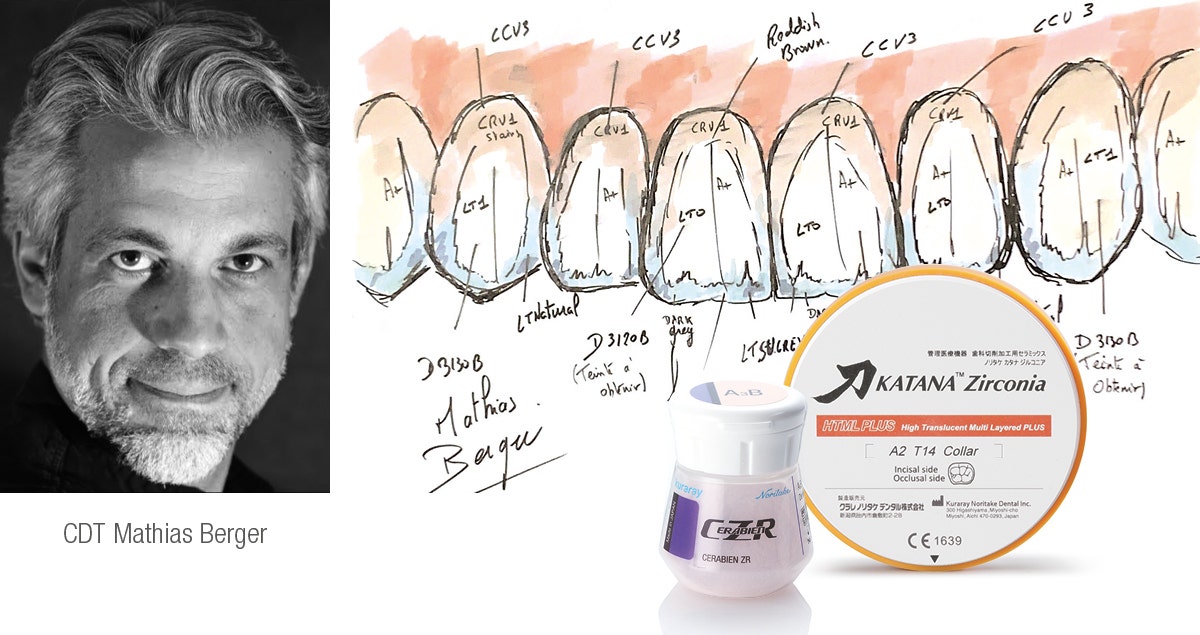
Fig. 1. Layering sketch for the restoration of a fractured central incisor in three layers: Layer one.
Fig. 2. Layering sketch for the restoration of a fractured central incisor in three layers: Layer two.
Fig. 3. Layering sketch for the restoration of a fractured central incisor in three layers: Layer three. After the first bake, small details were integrated, followed by a second bake. Finally, the restoration was finished with CERABIEN™ ZR FC Paste Stain and Glaze.
Fig. 4. Treatment outcome able to restore not only the smile, but also the self-confidence of the young girl.
Fig. 5. Immediately after cementation of the restoration, the restoration is barely identifiable, only the soft tissue needs some time for recovery.
ASPECTS TO BE CONSIDERED
But how to proceed in restoring single central incisors in the best possible way? The success of this type of restoration is hidden in the shape, which is the most difficult part. Managing to create a natural morphology is more than half the battle. The other important part is colour. The key to reproducing colour is in understanding how the utilized porcelains work. It is all about light reflection, absorption, translucency and opalescence, value and characteristic details. The more you gain experience and understand the optical properties of teeth and ceramics, the better your outcomes will be. Support is offered by a camera, a macro lens and a twin flash, which are used to capture and analyse the intraoral situation. For an initial analysis and understanding of shape and colour, I like to see the patients in my dental laboratory. Feeling the colour helps to develop the most realistic picture of what needs to be created. The key to successful realisation of the plan just developed is the use of reliable, easy-to-handle materials – in my case KATANA™ Zirconia and CERABIEN™ ZR Porcelains (both Kuraray Noritake Dental Inc.).
POSSIBLE STEPS
The first thing to focus on when starting to produce an anterior restoration – like in the case presented in figures 6 to 14 – is the correct value of the tooth. As soon as the framework or base is produced in the right value, you need to place what you see. Does the adjacent tooth show mamelons, traces of blue and orange? Those characteristics simply need to be observed and copied. There is no need to create something fancy. The tricky part is to use the available space reasonably. When there is plenty of space for the porcelain, it may be challenging to keep the value of the framework and avoid a greyish appearance. Depending on the die colour, age of the patient, natural surface texture and space available, an appropriate layering approach and finishing technique may be selected.
Fig. 6. Replacement of an anterior crown: Prepared tooth with severe discolouration. The adjacent central incisor has a special shape and vivid inner colour structure.
Fig. 7. Framework made of KATANA™ Zirconia ML in the shade A3. The target shade being A3.5, a quite opaque material was selected in a slightly brighter shade to achieve the required masking effect.
Fig. 8. Single-bake layering procedure: Application of CERABIEN™ ZR Opacious Body, …
Fig. 9. … Cervical Body, …
Fig. 10. … Body and Transitional Body.
Fig. 11. Incisal cut-back …
Fig. 12. … and creation of the mamelon structure.
Fig. 13. Application of Aqua Blue 1 …
Fig. 14. … followed by T Blue …
Fig. 15. … and Luster Porcelains.
Fig. 16. Halo effect created with Body.
Fig. 17. Treatment outcome. (After a first bake followed by minor adjustments, a second bake, surface texturing and glazing with CERABIEN™ ZR FC Paste Stain Clear Glaze.)
CONCLUSION
Creating a single central takes us out of our comfort zone. By paying attention, observing the adjacent teeth carefully and using materials we really understand, it is possible to meet or exceed our patients’ expectations. While specific tools like cameras and experience with the utilized materials offer support in producing predictable outcomes, my main credo is “If you want things around you to change, you must first change yourself”. For continued improvement, it is thus necessary to focus on professional growth and advancement. With the right mentors who will teach us the secrets of stratification and inspire and motivate us to continue advancing, it becomes easier to restore the smiles and self-confidence of our patients every time they need us to.
Acknowledgements
Special thanks go to the dental practitioners who treated the patients presented above – Andreas Skyllouriotis DDS, MSD, Surgically-Trained Prosthodontist, and Theo Odysseos, DDS, Diplomate, American Board of Oral Implantology / Implant Dentistry.
Dental Technician:
VASILIS VASILIOU
Vasilis Vasiliou was born in Nicosia, Cyprus, and graduated from the Technical School for Dental Technicians in Athens in 2004. He has furthered his education by attending several advanced seminars led by mentors and experts in the field, such as Ilias Psarris and Nondas Vlachopoulos.
Throughout his career, Vasilis has made significant contributions to the dental community, including presenting at various conferences in Greece and publishing articles in Greek dental magazines. Since 2020, he has been a key opinion leader for MPF Brush Company and, since 2022, a HASS Ambassador. Vasilis has been an active member of the International Team for Implantology (ITI) since 2019.
Together with his father, Vasilis runs a successful dental laboratory in Nicosia, specializing in all-ceramic and implant restorations. His extensive experience and commitment to excellence have established him as a respected professional in his field.