Case by CDT Daniele Rondoni and MDT Roberto Rossi
Working with high-translucency, multi layered zirconia (KATANA™ Zirconia Multi-Layered series from Kuraray Noritake Dental Inc.) paves the way toward indirect restorations that are closely adapted to our patients’ needs. Reduced wall thicknesses allow for minimally invasive tooth preparations, while polished zirconia in the occlusal contact areas provides for an antagonist-friendly behaviour. All this is possible due to the high aesthetic potential and homogeneous structure of the materials, which work well with a full-contour design or slight vestibular cutback. For individualization or characterization, different options are available. The portfolio of finishing solutions from Kuraray Noritake Dental has just been complemented by Esthetic Colorant for KATANA™ Zirconia, a set of twelve dyeing liquids for the company’s multilayered zirconia. They are applied to the milled restoration surface prior to sintering.
Some readers may wonder why there is a need for effect liquids applied to pre-shaded zirconia with a multi-layered colour structure. Being aware of natural teeth’s unique play of colours stemming from the shape and shade of the dentin core, however, the reason is quite obvious: Esthetic Colorant diffuses into the zirconia structure, hence allowing us to create depth effects even in monolithic restorations. Moreover, it enables the user to pre-treat tissue areas, and even by using the liquids on cutback designs, we are able to reproduce case-specific internal optical characteristics quite easily. Our standard approach for the use of Esthetic Colorant on KATANA™ Zirconia HTML Plus is described by means of the following case example: An implant- and tooth-based twelve-unit bridge with a slight vestibular cutback design, finished with Esthetic Colorant and CERABIEN™ ZR Porcelain.
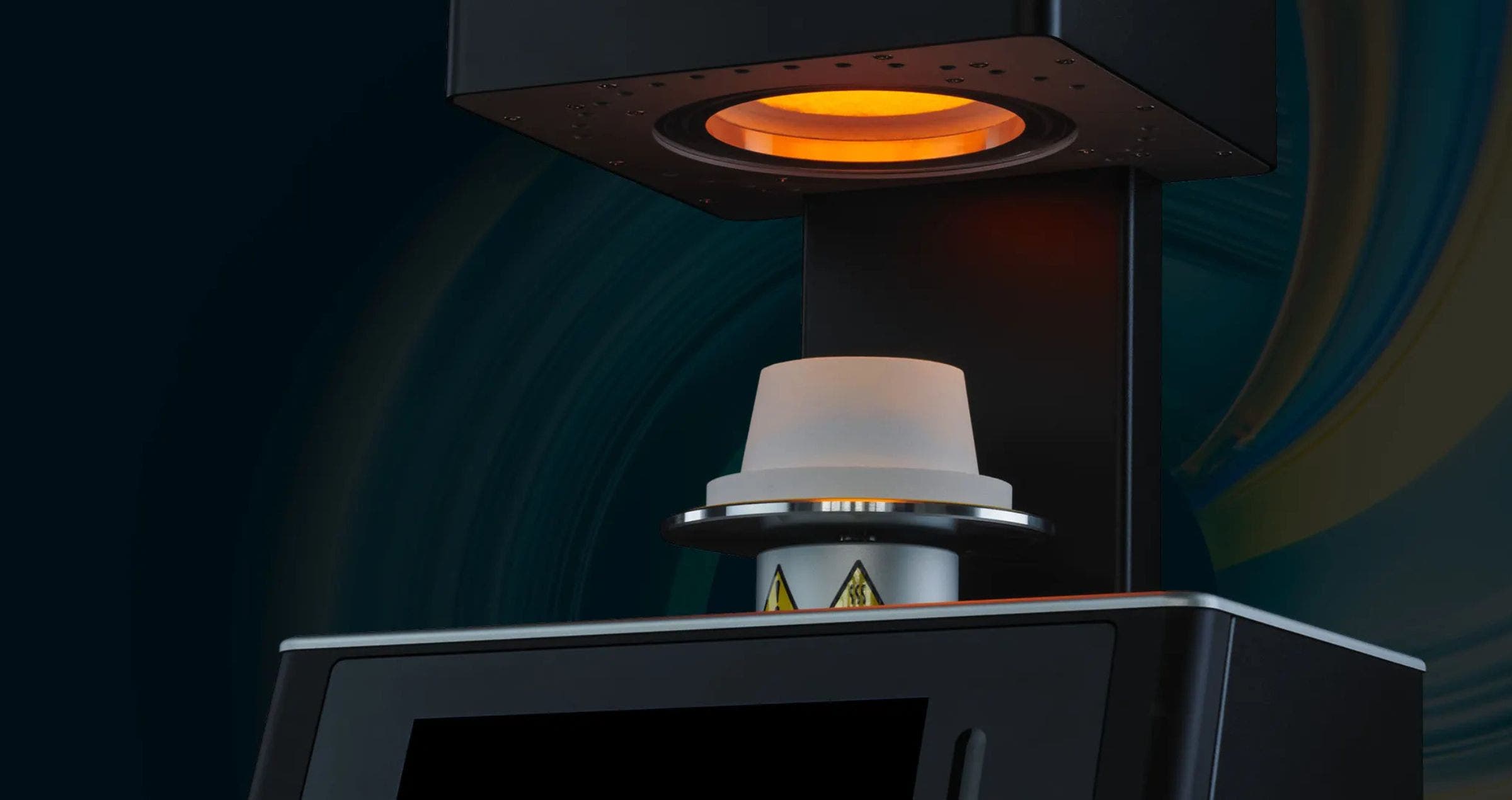
Fig. 1. Restoration with sintering support removed from the blank.
Fig. 2. Esthetic Colorant for KATANA™ Zirconia: Available shades.
Fig. 3. Frontal view of the milled restoration after the application of Esthetic Colorant. A chromatic map is not needed since the colours of the applied liquids are clearly visible.
Fig. 4. Occlusal view of the milled restoration after the application of Esthetic Colorant. The liquids were applied with the Liquid Brush Pen for Esthetic Colorant.
Fig. 5. Frontal view: Appearance of the restoration after sintering.
Fig. 6. Occlusal view: Appearance of the restoration after sintering.
Fig. 7. Beautiful translucency and mamelon structures in the incisal area.
Fig. 8. Situation after the application of a thin layer of CERABIEN™ ZR Porcelain, which creates an enamellike window effect and reveals the play of colours found underneath.
Fig. 9. Restoration after firing and glazing.
FINAL SITUATION
Fig. 10. Beauty shots…
Fig. 11. … of the final restoration.
Easy handling and application, impressive colour effects: Esthetic Colorant perfectly fits into our micro-layering approach with a cutback design adjusted to the age and needs of every patient. Being applied on the pre-sintered zirconia surface, the liquids do not require any extra heat treatment – the restoration is simply dried and then sintered as usual. Esthetic Colorant may be used instead of or in combination with internal stains, luster porcelains and liquid ceramics – whatever complements a laboratory’s existing approach to highly aesthetic zirconia restorations.
Dentists:
| CDT Daniele Rondoni | MDT Roberto Rossi |