Sementering av indirekte restaureringer
Noen selskaper gjør hovedsaklig bruk av grunnleggende teknologier som er utviklet av andre for å forbedre produktene sine og lansere nye, mens andre produsenter utfører grunnleggende forskning og teknologiutvikling i egen bedrift. Er denne forskjellen relevant for dem som gjør daglig bruk av de resulterende produktene på tannklinikken eller på det tanntekniske laboratoriet? Vi mener det, siden produsenter med en dypere forståelse for de underliggende komponentene, kjemien og teknologiene er i stand til å løse utfordringer og respondere på brukernes behov raskere og mer fleksibelt. Artikkelen beskriver påvirkningen som flere grunnleggende teknologier utviklet av Kuraray Noritake Dental Inc., har hatt på sementeringen av indirekte restaureringer.
Adhesiv sementering før og nå
Muligheten for å frese dentale restaureringer av diverse keramer har åpnet nye muligheter innen protetikken. Svært estetiske restaureringer kan fremstilles og sementeres. Noe som ofte undervurderes i denne sammenhengen, er den rollen som adhesive sementer spiller. Ikke bare muliggjør de translucente, estetiske, tannfargede restaureringer, men de baner også vei for mindre invasive prepareringer og design av restaureringer. Tidligere systemer for adhesiv sementering med kjemisk binding mellom tann og restaurering hadde dessverre dårlige langtidsresultater og høy teknikksensitivitet, samtidig som arbeidsprosedyren var ekstremt komplisert. Teknologi som er utviklet av Kuraray Noritake Dental Inc., har gjort signifikante bidrag til bedre langtidsresultater og forenklet arbeidsprosess.
Optimalisering av langtids bonding-resultater
For å oppnå bedre langtidsresultater av tidlige bondingprosedyrer (spesielt til dentin), bestemte Kuraray, en forløper for Kuraray Noritake Dental Inc., seg for å fokusere på utviklingen av en kraftigere adhesiv monomer på 1970-tallet. Det første trinnet på utviklingen som ledet frem til suksess, var introduksjonen av fosfat-monomeren Phenyl-P i 1976. Fem år senere, etter fortsatte anstrengelser for å forbedre og raffinere molekylstrukturen, kunne man så introdusere den poulære MDP monomeren som er i stand til å gi sterk og holdbar binding til emalje, dentin, metaller og zirkonium.
Det faktum at MDP monomeren fremdeles inngår i alle adhesiver og adhesive sementeringssystemer fra Kuraray Noritake Dental Inc., og i mellomtiden er tatt i bruk av andre produsenter for å optimalisere bindingsstyrken og holdbarheten på bindingen for produktene, viser bare hvor genial denne oppfinnelsen var. I motsetning til MDP som er produsert andre steder, fremhever den Originale MDP seg takket være en renhet som ingen har kunnet matche. Studier viser at dette nivået på renhet har en positiv effekt på ytelsen1. Ved at den tilbyr stabilitet i fuktige omgivelser, har MDP monomeren bidratt til en mere konsistent ytelse for de produktene som inneholder den.
Ulike MDP monomerer har ulik renhetsgrad og ulik bindingsstyrke.
Tre eksperimentelle, selvetsende primere ble fremstilt. De inneholdt 15 vekt% 10-MDP som ble levert fra ulike kilder. KN (Kuraray Noritake), PCM (Tyskland) og DMI (Designer molecules Inc. USA). Data med tillatelse fra Dr. Kumiko Yushihara.
For at adhesive resinsementer skal kunne levere sterk binding og god marginal forsegling, er det imidlertid ikke nok å inneholde en adhesiv monomer. Effektiv
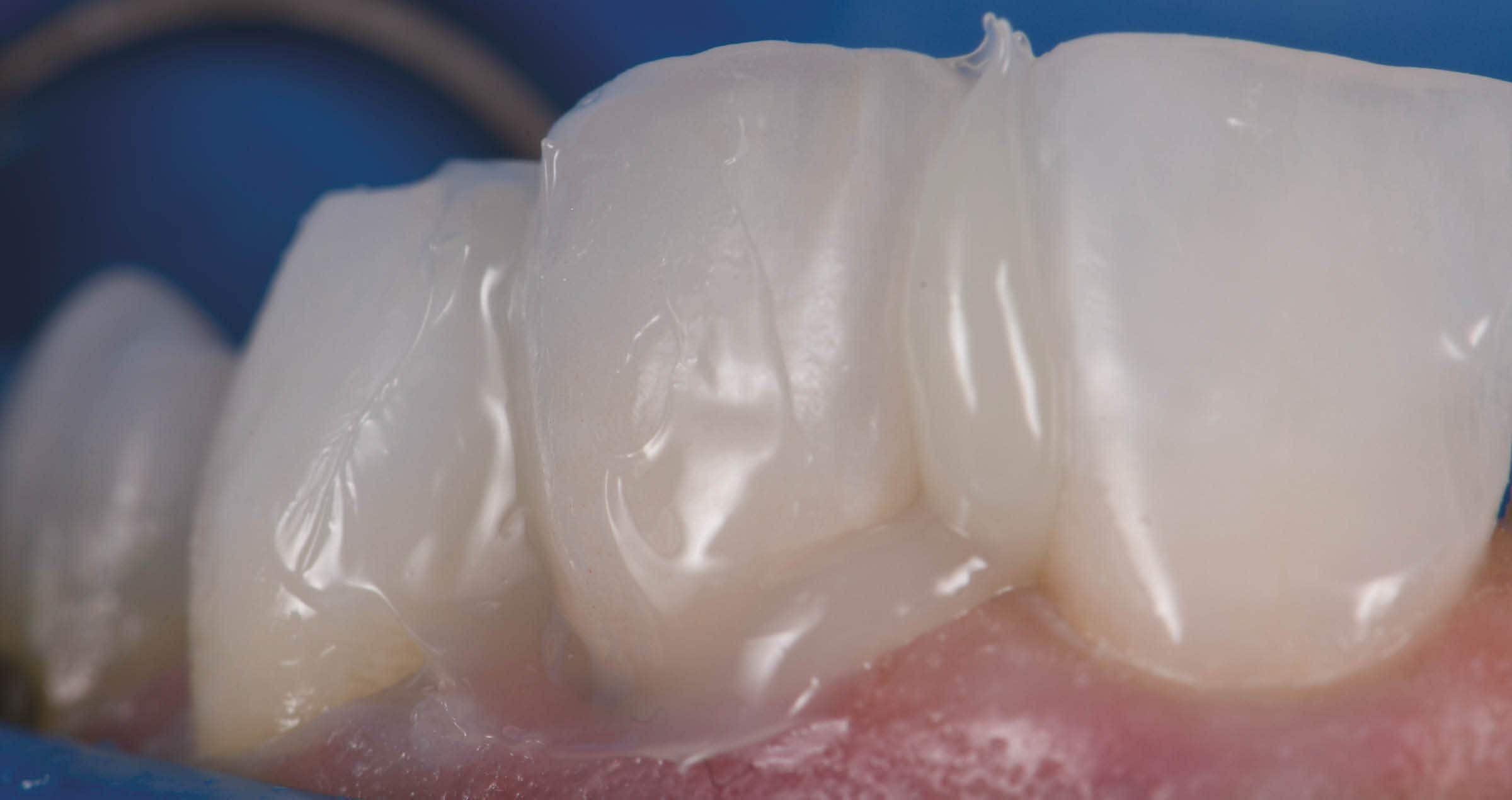
polymerisering av denne monomeren er også viktig- og dette er ikke alltid så lett å oppnå. For å kunne oppnå effektiv lysherding og kjemisk herding av PANAVIA™ V5, utviklet Kuraray Noritake Dental Inc. Touch-Cureteknologien. Nøkkelkomponenten i denne teknologien er en nylig utviklet, svært aktiv polymerisasjonsakselerator i PANAVIA™ V5 Tooth Primer som virker i samspill med den sure MDP monomeren. Straks sementen kommer i kontakt med den allerede primede tannoverflaten, starter polymeriseringen. I PANAVIA™ Veneer LC, en lysherdende sement som bruker desamme primerne, får vi samme virkningsmekanisme. Polymeriseringen starter umiddelbart i kontaktsonen mellom sement og primet tann, mens PANAVIA™ Veneer LC sementpastaen har den egenskapen at den har lang arbeidstid i rombelysning og polymeriseres ved lysherding.
For eksempel ble dette fenomenet evaluert for PANAVIA™ F2.0., forgjengeren til PANAVIA™ V5. Resultatet av studien var at PANAVIA™ F2.0 viste mye bedre marginal forsegling enn andre sementer som ble testet2. Denne dokumenterte, sikre forseglingen av spalten fører til lavere marginal lekkasje, til en høy polymerisasjonsgrad selv i selvherdende modus (uten lysherding eller hvor lyset fra herdelampen er blokkert), og derfor til en spesielt sterk binding.
En annen fordel ved å inkorporere av polymerisasjons-akseleratoren, er at den virker som et sterkt reduksjonsmiddel. Det nøytraliserer natrium-hypokloritt som er hyppig brukt som irrigasjonsmiddel ved endodontisk behandling, slik at den negative påvirkningen dette stoffet har på bindingsstyrken til senere anvendt sement elimineres.
Forenkler sementeringen av glass-keramikk
Færre flasker, færre trinn og strømlinjeformede sementeringsprosedyrer: Dette er grunnen til at selv-adhesive resinsementer har blitt utviklet og introdusert fra tidlig på 2000-tallet. De fleste av disse produktene har imidlertid et begrenset indikasjonsområde. De virker bra på zirkonium, metall, emalje og dentin, men de er enten ikke indisert, eller trenger en ekstra silan-primer, for bonding av glass-keramikk. PANAVIA™ SA Cement Universal, som inneholder MDP, er annerledes takket være en annen proprietær teknologi fra Kuraray Noritake Dental Inc.: LCSi monomeren, et silan -koblende middel med lang karbonkjede. Denne monomeren danner en sterk kjemisk binding med komposittresin, porselen og silikatkeramikk (som f.eks. litium disilikat). Slik elimineres behovet for en separat silankomponent (primer eller adhesiv). Ved å øke fordelene ved denne teknologien, skiller PANAVIA™ SA Cement Universal seg klart fra andre selv-adhesive resinsementer som en ekte én-komponent sement som også kan brukes til glass-keramikk.
Hvis ønskelig, kan produktets bindingsstyrke til tannen økes ved å bruke den populære universaladhesiven CLEARFIL™ Universal Bond Quick som inneholder Rapid Bond Technology. Denne teknologien har blitt utviklet av Kuraray Noritake Dental Inc. for å løse problemene som er relatert til den langsomme penetrasjonen av, særlig fuktig dentin, som kjennetegner universaladhesivene. For å oppnå skikkelig penetrasjon må disse adhesivene gnugges aktivt inn i tannen i lang tid, eller brukeren må vente en tid før lysherding. Rapid Bond Technology består av den originale MDP monomeren kombinert med hydrofile amid monomerer. Dette gjør at bondingen trenger raskt og dypt inn i fuktig dentin. Resultatet er kortere appliseringstid og enklere arbeidsgang uten at bindingsstyrken påvirkes negativt.
Konklusjon
Teknologier utviklet av Kuraray Noritake Dental Inc. har bidratt sterkt til forbedret bindingsstyrke ved adhesiv sementering og til at selvadhesive resinsementer virkelig har blitt egnet til universelt bruk.. Selskapet tilbyr et strømlinjeformet produktutvalg av høyeffektive resinsementer for alle brukere og for alle typiske kliniske kasus. Færre komponenter og færre trinn er nødvendige og prosedyrene er forenklet. Dette fører til færre feilslag og estetiske restaureringer med lang levetid. I tillegg til de teknologi-relaterte fordelene, tilbyr de nevnte produktene mange andre fordelaktige egenskaper. En detaljert beskrivelse finnes på kuraraynoritake.eu.
Referanser
*) Functional monomer impurity affects adhesive performance.; Yoshihara K, Nagaoka N, Okihara T, Kuroboshi M, Hayakawa S, Maruo Y, Nishigawa G, De Munck J,
Yoshida Y, Van Meerbeek B. Dent Mater. 2015 Dec;31(12):1493-501.
**) Touch-Cure Polymerization at the Composite Cement-Dentin Interface.; Yoshihara K, Nagaoka N, Benino Y, Nakamura A, Hara T, Maruo Y, Yoshida Y, Van Meerbeek
B.J Dent Res. 2021 Aug;100(9):935-94