By DT Simone Maffei and Dr. Filippo Menini
EVOLUTION IN PROSTHODONTICS
Nowadays, digital workflows in prosthodontics are well-established, and many modern dental laboratories have already embraced the option of producing monolithic restorations or restorations with a minimal cut-back for micro-layering in a fully digital environment.
The spread of digital technologies and the availability of new restorative materials with improved aesthetic properties have increased the popularity of this technique among dental technicians. This way of working offers considerable advantages for daily procedures, starting with improved ways of communication between the clinician and dental technician. For example, it is now possible to view and evaluate impressions with the whole treatment team including the dental technician almost instantaneously after impression taking – and without anyone having to leave their office.
In addition to advanced communication options, digital technologies have allowed us to use materials that otherwise could not be processed, such as zirconia and hybrid composites. As a consequence, lots of innovative materials conquered the market, and this has opened up the possibility to always select what is perfectly suited for each specific clinical situation. Adapting to these trends is absolutely essential for anyone who wants to meet a modern dental practitioner’s increased demands.
LONG DISTANCE DENTAL COLLABORATION
Working with digital workflows has allowed us to broaden the scope of action of the modern laboratory, enabling virtually effortless collaboration with clinicians hundreds or thousands of kilometres away. The case presented below is a perfect example: In our dental laboratory in Modena, we produced two anatomical crowns made of KATANA™ Zirconia for a patient who needed a combination of direct and indirect restorative treatment to be carried out by Dr. Filippo Menini in Belluno, about 300 km to the northwest. The whole communication and coordination between practice and laboratory was performed remotely and without us seeing the patient.
MATERIAL CHOICES
Monolithic restorations offer countless clinical and technical advantages. With a major part of the process accomplished by machines, they truly rationalize procedures. The challenge resulting from this simplification, however, lies in the achieving of excellent aesthetics.
Whereas until a few years ago, it was very difficult to accomplish this task due to the poor optical properties of the available materials, today we can safely say that we have materials, techniques and protocols at our disposal that allow us to obtain aesthetically acceptable results. At the same time, those materials offer excellent mechanical resistance to the forces and stress to which they are exposed in the oral cavity and a very high precision of fit, if these restorations are produced in a fully digital workflow.
We have chosen to work with prosthetic materials and finishing solutions from a company that manufactures and develops them in-house: Kuraray Noritake Dental Inc. (Kuraray Noritake). They offer zirconia discs for milling as well as effect liquids, veneering porcelain and liquid ceramics for an aesthetic finish and even resin cement systems for adhesive luting – all from a single source. This gives us the advantage of using clear and predictable working protocols from fabrication to cementation of the restoration.
CLINICAL CASE
The 31-year-old patient presented with multiple carious lesions, inadequate restorations and in particular a destructive caries in the maxillary right second premolar (tooth #15, FDI notation, Fig. 1). The latter tooth was endodontically treated and built up using a glass fibre post. The X-ray revealed carious lesions and infiltrated margins of the restorations (Fig. 2). The treatment plan for this quadrant included direct composite restorations on the first premolar and first molar (teeth # 14 and 16) and an indirect zirconia crown used to restore the second premolar (tooth #15; Fig. 3). In addition, a zirconia crown needed to be produced for the mandibular right second premolar (tooth #45).
Fig. 1. Initial clinical situation in the maxillary right quadrant.
Fig. 2. Radiograph showing carious lesions and restorations with marginal leakage.
Fig. 3. Marked surfaces that will be treated.
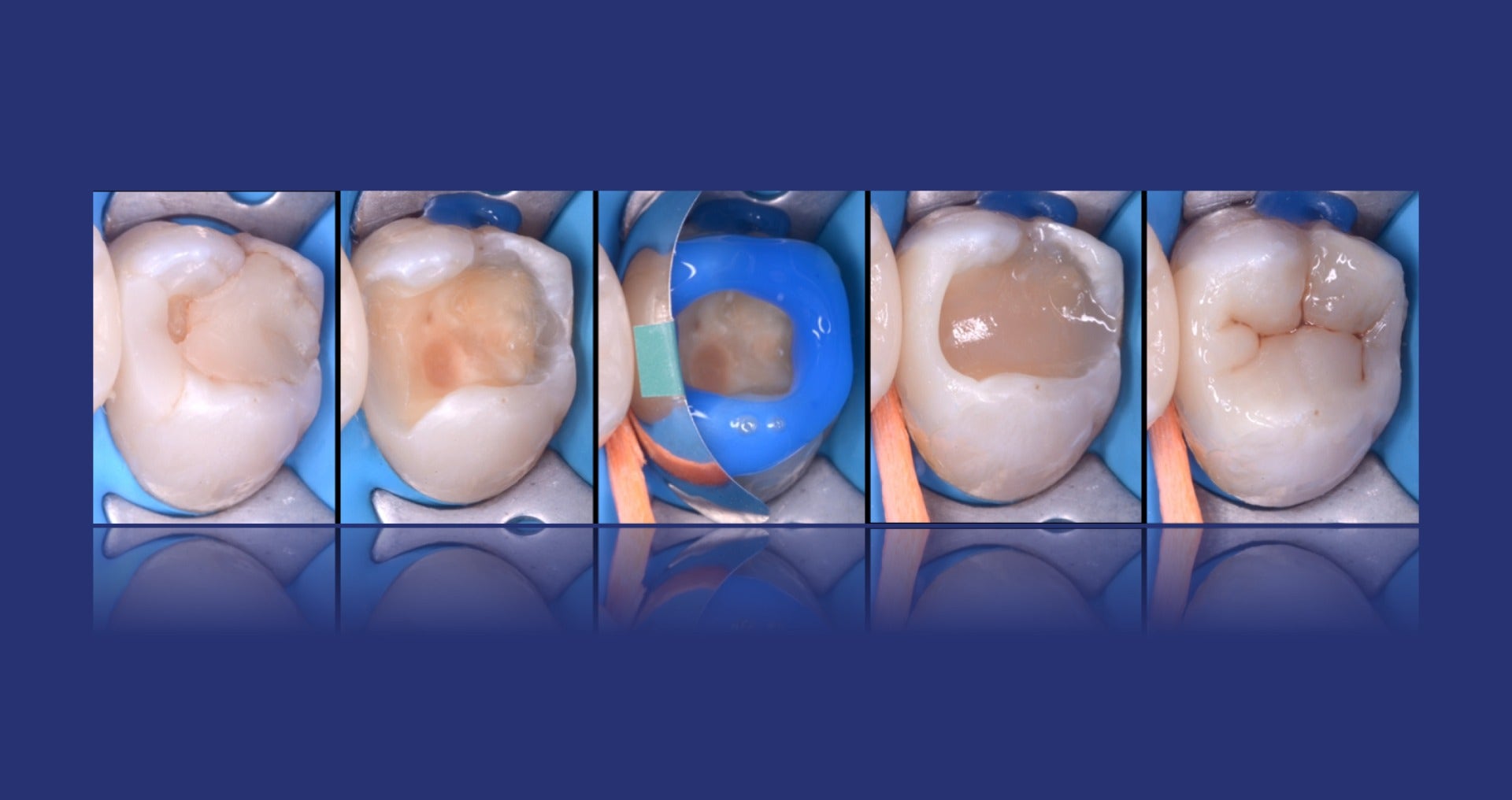
During the first session, the clinician restored the first molar and premolar with composite (Figs. 4 and 5). In addition, the tooth preparation on the maxillary and the mandibular second premolar was performed using the biologically oriented preparation technique (BOPT; Figs. 6 and 7). Two single-tooth temporaries were then produced, recreating a cervical profile according to the BOPT (Fig. 8). In the next step, the digital impression was taken using the double chord technique (Fig. 9). The file generated by the intraoral scanner was first analysed using a greyscale view. This view allows for a better assessment of the quality of the acquired data than the coloured image (Fig. 10). The temporary restorations were finished, polished and placed on the teeth using temporary cement (Fig. 11).
Fig. 4. Restoration procedure on the maxillary first molar.
Fig. 5. Restoration procedure on the maxillary first premolar.
Fig. 6. BOPT crown preparation on the maxillary second premolar.
Fig. 7. Detail of the subgingival preparation, using burs with calibrated notches, taking care not to touch the supra-crestal attachment complex, but precisely taking care to remain within the width of the sulcus.
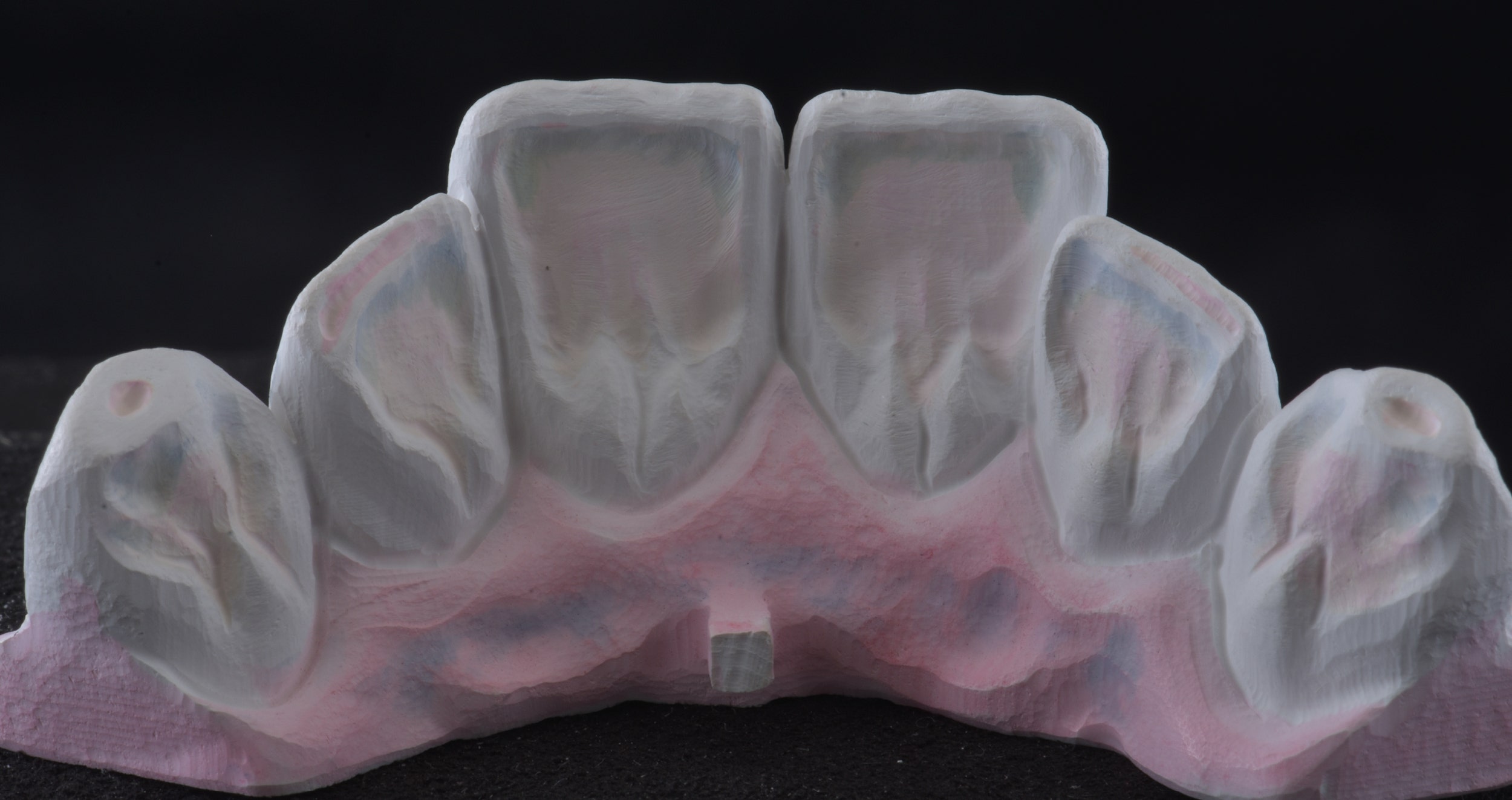
In the dental laboratory, we received the intraoral scans in the STL format: Both arches with the prepared teeth and the usual bit register (vestibular scan of the arches in occlusion). Following a careful evaluation of the impressions and the quality of the triangulation of the points of the STL file detected by the scan, a full-contour design of the crowns was performed (zero cutback crowns). This allows us to obtain an emergence profile, according to the BOPT, which is extremely accurate. The anatomy was developed taking into account the functional movements of the patient, which were based on information retrieved from a virtual articulator integrated in the CAD software. These movements can be verified and – if necessary – corrected on the physical articulator in a subsequent step. As it is possible to use the same type of articulator (in our case ARTEX by Amann Girrbach) both in the virtual environment and the real one (control phase) offers the advantage of using the same settings and consequently the same movements in both worlds (Fig. 12).
Fig. 8. Production of the temporary restoration.
Fig. 9. Digital impression taken using the double cord technique: a 000-sized cord soaked in aluminium chloride is placed in the sulcus as the first cord, followed by a non-soaked cord of size 1.
Fig. 10. Greyscale view of the impression, facilitating the clinical evaluation.
Fig. 11. Cementation of the temporary restoration.
Fig. 12. Virtual models based on the digital impression of both arches, with the software-designed full-contour crowns in different views.
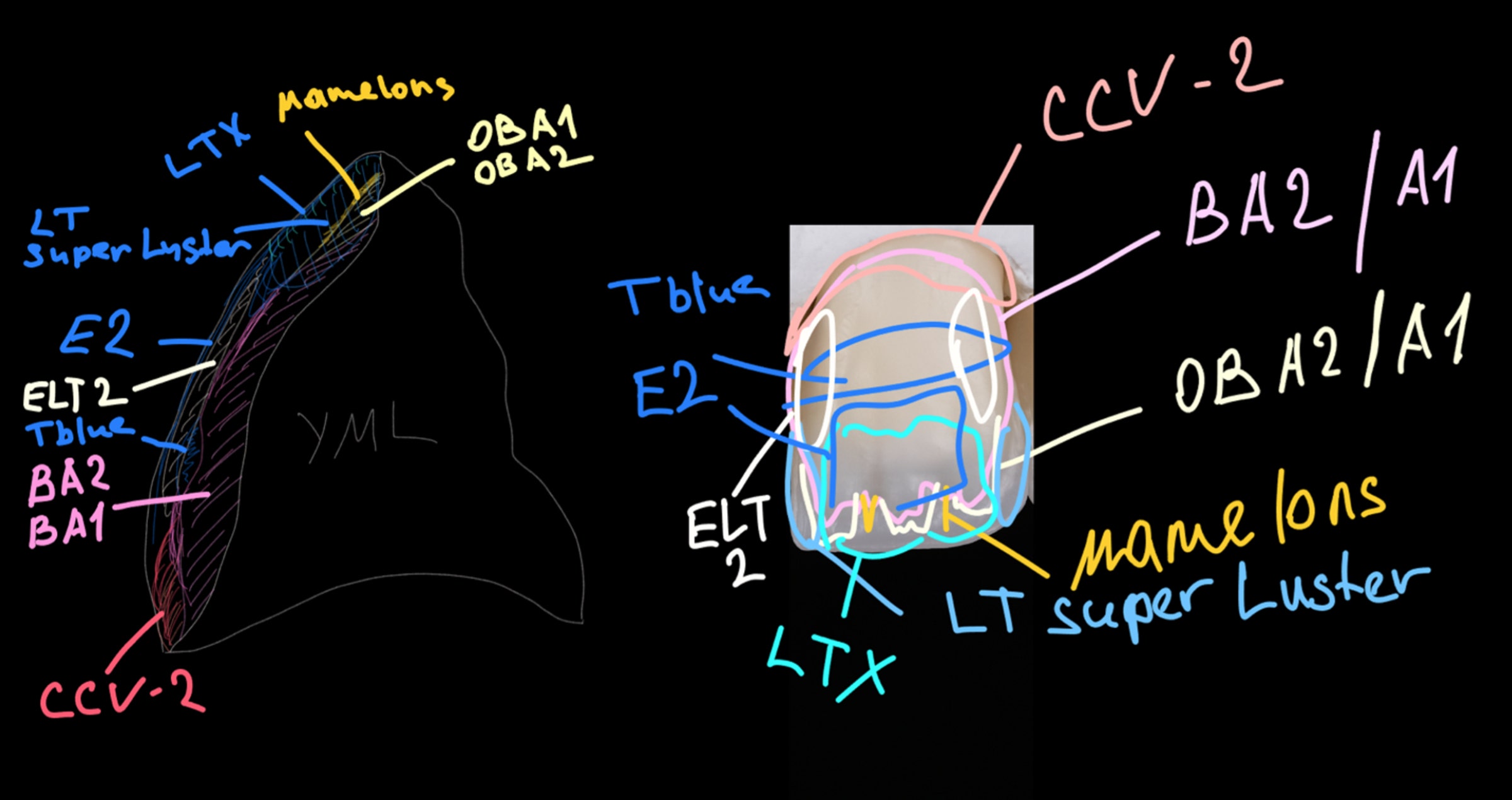
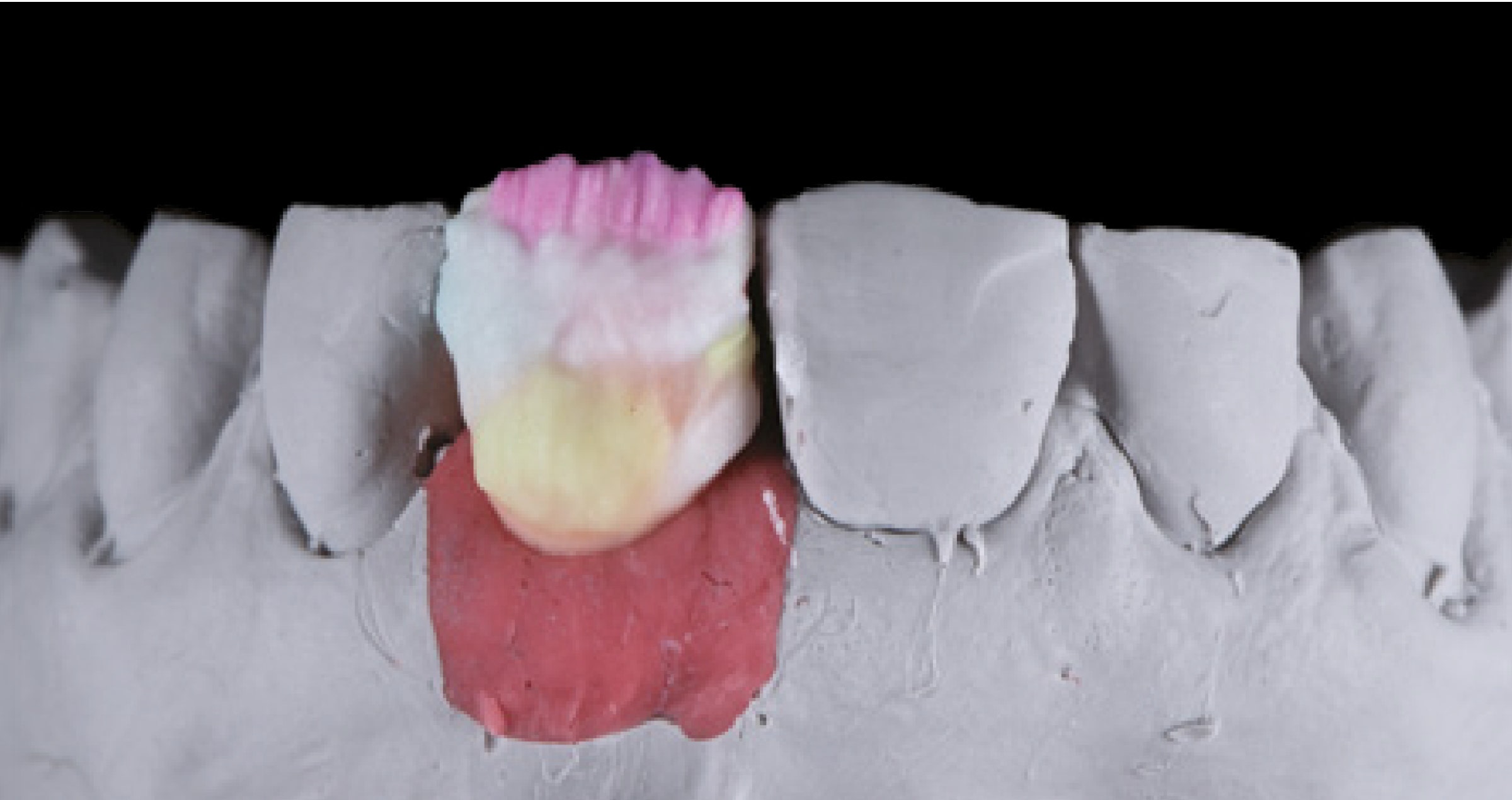
The STL files of the designed restorations were sent to the CAM software for milling of the zirconia crowns with a 5-axis CNC machine. The material of choice was in this case KATANA™ Zirconia YML (Kuraray Noritake Dental Inc), which is multi-layered in strength, translucency and colour, and thus suitable for a variety of cases (Fig. 13). Once milling was finished, the elements were removed from the disc and their surface treated with diamond burs and specific rubbers designed for the processing of pre-sintered zirconia. In this phase, it is possible to individualise the anatomy and surface texture of the restorations, a task that is very difficult to accomplish in the milling process. With the dedicated rubbers, the surface can also be smoothened, which will improve the appearance of our restorations after sintering (Fig. 14).
On top, individualization of the pre-sintered restorations was accomplished with Esthetic Colorant (Kuraray Noritake). These new effect liquids have been specifically developed for KATANA™ Zirconia. They contain a special primer that limits the depth of penetration, which results in an appearance similar to external stains, while a depth effect is created. Precise application of the liquids is possible with the Liquid Brush Pen. The Esthetic Colorant line-up consists of twelve colours to facilitate stock management in the dental laboratory, while still providing for natural aesthetics and perfect harmony in the oral cavity. Impact on the flexural strength of the zirconia substructure by the liquids is kept to a minimum, as they have been optimised to limit this effect and avoid fractures. (Fig. 15).
Sintering is carried out in a specially calibrated furnace, scrupulously following the protocol recommended by the manufacturer. Afterwards, the finishing procedure can be continued. With special stones, the cervical edge was first regularised: In the deeper, subgingival areas, the intraoral scanner usually has some difficulties capturing all the necessary information. As a consequence, the STL file is triangulated with some irregularities at the cervical margin. These irregularities need to be regularised, before the thickness of the margin is reduced to '0'. In fact, during milling it, is created with a thickness of 0.2 mm to avoid micro-chipping that would compromise the accuracy of the cervical margin. Figure 16 shows both the thickness of the cervical margin, which, despite the finishing preparation, retains a thickness of 0.2 mm, and the irregular course of the same due to the irregular shape of the STL file around the sulcus.
Fig. 13. KATANA™ Zirconia YML blank with milled crowns.
Fig. 14. Finishing with diamond burs and specific rubbers for pre-sintered zirconia.
Fig. 15. Individualisation with Esthetic Colorant.
Fig. 16. Finishing of the restorations after sintering.
The restorations were then sandblasted with 50-μm aluminium dioxide at 2 bar pressure and cleaned under a steam jet. After an evaluation of the colour revealed after sintering, the finishing phase was completed with the aid of CERABIEN™ ZR FC Paste Stain (Kuraray Noritake Dental Inc.) and polishing instruments. The ceramic emulsions FC Paste Stain allow us to adjust the chroma and value of the restorations and to imitate all those aesthetic features that will improve integration in the oral cavity. With this technique, it is very easy to achieve the desired shade match, as the appearance of the stain applied to the surface is exactly like its appearance after firing. In this way, it is easy to monitor the outcome and – if desired – compare with a reference and adjust whenever necessary (Figs. 17 and 18).
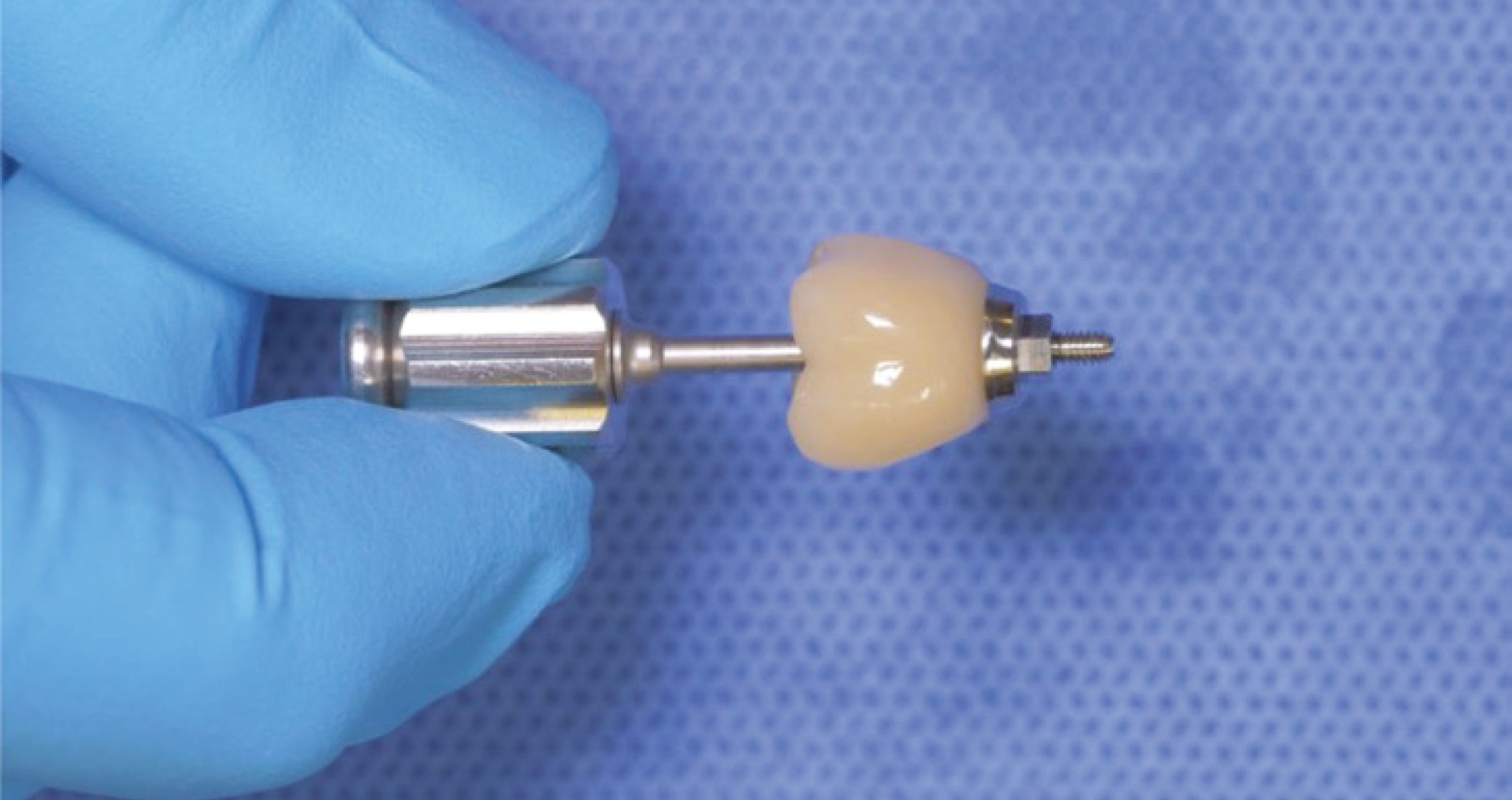
For cementation of the restorations, the clinician used PANAVIA™ SA Cement Universal in combination with KATANA™ Cleaner (both Kuraray Noritake Dental Inc.). The cleaner has a pH value of 4.5 be used both intra and extra-orally, improving adhesion in all restorative procedures. PANAVIA™ SA Cement Universal is the only self-adhesive resin cement containing the unique LCSi monomer – a long carbon-chain silane coupling agent. In combination with the original MDP monomer, which is also present in the paste and enables chemical adhesion with zirconia, dentin, enamel and metal alloys, this coupling agent provides for adhesion of the cement to any material, including glass-ceramics, without the need for a separate primer (Figs. 19, 20 and 21). At the cementation appointment, the last planned direct reconstruction of the maxillary second molar (tooth #17) was also carried out.
Fig. 17. Characterisation with CERABIEN™ ZR FC Paste Stain.
Fig. 18. Finished restorations ready to be handed over to the clinician.
Fig. 19. Cementation procedure in the maxilla: Sandblasting of the tooth and cleaning of the tooth structure with KATANA™ Cleaner.
Fig. 20. Cementation procedure in the maxilla: Sandblasting of the crown’s intaglio and cleaning of the restoration with KATANA™ Cleaner.
Fig. 21. Cementation procedure in the maxilla: Self-adhesive cementation with PANAVIA™ SA Cement Universal.
Fig. 22. Direct restoration procedure on the second molar.
Fig. 23. Restorations immediately after finishing and polishing.
Fig. 24. Detailed view of the restored quadrant.
Fig. 25. Occlusal view of the maxillary teeth.
RESULT
The aesthetic integration provided by the high quality of KATANA™ Zirconia YML, combined with the pre- and post-sintering individualisation, made it possible to achieve an excellent integration of the anatomical zirconia crowns. Figures 22 to 25 show the outcome in the newly restored maxillary right quadrant with natural tooth structure, direct composite restorations and the monolithic zirconia crown.
ABOUT THE AUTHORS
DT SIMONE MAFFEI
Simone Maffei, a dental technician since 1996 (IPSIA L.Galvani Reggio Emilia), embarked on his career in Modena at his father William's laboratory. Throughout his professional journey, he has demonstrated a commitment to excellence by participating in numerous courses led by prominent international speakers. These courses span the realms of dental technology and photography. Presently, Maffei is not only a respected speaker at national and international conferences but has also contributed articles to both Italian and foreign sector magazines. His written works delve into the intricate intersection of dental photography and the aesthetics of the smile. A testament to his expertise, Maffei earned recognition as the recipient of the prestigious AIOP International Award in 2014. He actively shares his knowledge by conducting courses in Italy and abroad, focusing on dental technology, dental photography, natural ceramic layering techniques, and the three-dimensional coloring of monolithic restorations. As a valued member of the Digital Dental Revolution (DDR) Team, Maffei serves as a speaker at courses and international conferences, where he imparts insights on various facets of digital dentistry. Simone Maffei is also the proud owner of the Laboratorio Odontotecnico Maffei in Modena. Collaborating with his sister Elisa, the laboratory specializes in crafting aesthetic ceramic reconstructions for both natural teeth and implants, showcasing a dedication to the art and science of dental aesthetics. Active Member of AIOP SOSPESO – Accademia Italiana di Odontoiatria Protesica (Italian Academy of Prosthetic Dentistry). Ordinary Member of SIPRO Società Italiana Protesi e Riabilitazione Orale (Italian Society of Oral Prosthetics and Rehabilitation).
FILIPPO MENINI
Dr. Filippo Menini graduated in Dentistry and Dental Prosthetics from the Universidad Europea De Madrid in 2017. He has been passionately dedicated to the study of direct and indirect adhesive techniques in the field of conservative dentistry. He became a Regular Member of the Italian Academy of Conservative Dentistry in 2018 and the Italian Academy of Prosthetic Dentistry in 2019. In November 2021, he joined the Think Adhesive Members, and since February 2022, he has been a contract tutor at the University of Siena in the Endo-Resto master program taught by Professor Grandini. Dr. Menini has attended numerous courses in conservative dentistry, endodontics, periodontology, and adhesive prosthetics to manage his work in a multidisciplinary perspective. He has his dental practice in Belluno.