No shade taking needed. Just one shade to cover all posterior cases. Even the larger Class I's and II's!
Blog
A guideline with regard to contemporary materials
The retention of the fixed prosthodontic restorations is a critical factor for the long-term success, as the loss of crown retention is one of the main reasons for failure of crowns and fixed dental prosthesis (FDP) (1, 2). There are three main elements that need to be considered to achieve proper retention of the restorations; the tooth preparation, the restorative material and the luting agent.
TOOTH PREPARATION
During tooth preparation there are some important features to be considered, such as the height, angle and surface texture of the abutment tooth, in order to achieve an adequate retention and resistance form which provide stability of the restorations to resist dislodgment and subsequent loss (3). Retention form is responsible for counteracting tensile stresses, whereas resistance form counteracts shear stresses (4).
In order to achieve a sufficient retention and resistance form for full coverage crowns it is recommended that the height of the abutment tooth should be at least 4 mm and that the optimal convergence angle should range from 6 to 12 degrees with a maximum of 15 degrees (1, 5-8).
RESTORATIVE MATERIAL
With the continuous introduction of new restorative materials to the dental market it is important to take into consideration the different mechanical properties of the various materials. The composition and the surface properties of the material have a decisive role in the ability to accomplish mechanical and/or chemical attachment to the restoration and therefore achieving required retention.
LUTING AGENT
The luting agent is the connection between the tooth and the restoration. Proper luting of indirect restoration is critical in achieving long-term success as it highly influences the retention of the restoration as well as tightly sealing the gap between the restoration and the tooth. Although there are several classifications for the definitive luting agents, they can be , however, classified into two main categories based on the ability to achieve chemical connection to different substrates; conventional (e.g. zinc phosphate, glass-ionomer and resin-modified glass-ionomer cements) and adhesives. Most commonly used and best documented adhesive luting agents are the adhesive composite resin cements.
Composite resin cements can be further classified according to the chemical composition into traditional full-adhesive resin cement and self-adhesive resin cements, both also differ in the bonding procedure. The full-adhesive resin cements require pre-treatment of the tooth structure and restorative material using separate adhesive systems. In this combination of the resin cement and the adhesive system, very durable chemical bonding can be reached.
To simplify the luting procedure and eliminate the need of using several components, the self-adhesive resin cements are a good choice for the daily busy practice, in which reliable bonding can be achieved in only one simple step of cement application, mostly without additional primers or bonding agents.
With the availability of different types of cements, the decision of choosing the suitable luting agent and method can be confusing for the practitioner. Especially with the wide use of contemporary restorative materials such as new generations of highly translucent zirconia as well as reinforced-composites, it is important to take into consideration that the properties of such materials differ highly from metal or earlier generations of zirconia. Subsequently the choice of the luting agent must be appropriate to achieve satisfying results and long-term success. Therefore, in this article, the authors aim to provide insights for the clinicians on choosing the correct luting agent that can help achieve satisfactory results for the dentist as well as the patients.
CONVENTIONAL CEMENTATION OR ADHESIVE LUTING?
The choice of whether to use a conventional cement or an adhesive resin cement depends on several factors, the key factors are:
- Retention and resistance form of the abutment tooth.
- Mechanical and optical properties of the restorative material (flexural strength and translucency).
- Simplicity of the workflow and special requirements of the working environment.
1) RETENTION AND RESISTANCE FORM OF THE ABUTMENT TOOTH
Minimal-invasive restorations, such as resin-bonded FDP, labial and occlusal veneers and inlay-retained FDP are based on a non-retentive preparation form. In this case the only possible method to achieve retention is the adhesive luting (9-11).
Even though such preparations completely lack a retentive form, long-term success of the restorations is well-documented when using a durable resin cement (e.g. PANAVIA™ 21, Kuraray Noritake Dental Inc., Japan) and proper bonding procedure (10, 11).
For full-coverage restorations (e.g. crowns and FDPs), the guidelines for tooth preparation discussed before (minimum height of 4 mm and maximum convergence of 15 degrees) need to be applied in order to achieve the retention and resistance form required to make cementation with a conventional luting agent acceptable.
However, in reality this retention form is hard to realize due to several factors.
In cases of severe loss of tooth substance, achieving a minimum height of the abutment tooth is only possible with building up the tooth using a core build-up material which in some cases can be considered time consuming especially when the required build-up is minor (for example 1-2 mm). Moreover, increasing the height through core build-up is sometimes not possible, as in cases with short clinical crowns and insufficient occlusal clearance that is essential to provide the minimum thickness required for the restorative material. In such cases surgical crown lengthening is necessary to increase the height of the tooth without compromising the occlusal space required, which can be time consuming for the clinician and undesirable for the patient as it involves a surgical procedure and extends the treatment process.
Concerning the convergence angle, several studies showed that in reality and in daily practice of the dentist, the preparation angle is much higher than 15 degrees (5, 6, 12, 13). For instance, preparations from general practitioners were evaluated digitally and compared to clinical recommendations and it was found that the mean convergence angle was 26.7 degree with the distopalatal angle being 31.7 degree (12).
Based on the previous concerns, it can be concluded that achieving a proper retention form during daily practice is hard to realize and thus conventional cementation in such cases can present clinical problems especially on the long term. Therefore, adhesive luting can be recommended in these cases as an alternative to conventional cementation (6, 14). For full-coverage restorations with preparation designs featuring at least some mechanical retention, the use of self-adhesive resin cements can be considerate a good alternative as it provides high clinical success rates (9, 15).
Conclusion / Clinical Significance:
- For non-retentive minimal-invasive restorations, traditional full-adhesive luting is a must.
- For full-coverage restorations, full-adhesive or self-adhesive luting is recommended.
- In case a retentive preparation with minimum height of 4mm and convergence angle of 6-12 degrees, adhesive luting as well as conventional cementation can be used.
2) MECHANICAL AND OPTICAL PROPERTIES OF THE RESTORATIVE MATERIAL
Flexural strength and translucency of the restorative material are critical factors that influence the decision which luting agent to use.
a) Flexural strength
As a general guideline for all-ceramic restorations, ceramics with low and medium flexural strength under 350 MPa should be adhesively luted with composite resin cements, as these restorations rely on resin bonding for reinforcement and support (9, 14, 16). This includes feldspathic-, glass-, hybrid-ceramics and composite.
Although discussions on conventional cementation versus adhesive luting for high-strength ceramics with flexure strength of more than 350 MPa have been going on for a long time (9), there are several studies showing an increased stability and strength of all types of ceramics, even lithium disilicate and zirconia, when they are adhesively luted (9, 17-20).
It is also important to consider that the documented success of most conventional cements is mainly combined with restorations made of metal or early generations of zirconia. Nonetheless, the clinical success of new generations of high-translucent zirconia can be significantly influenced by the luting agent as these new generations have notably lower flexural strength (9). And therefore, attention has to be paid to minimal material thickness together with adhesive luting to ensure long-term clinical success and prevent fractures (9).
Conclusion / Clinical Significance:
- For glass-ceramic, hybrid-ceramics and composites, adhesive luting is a must.
- For lithium disilicate and zirconia restorations, adhesive luting is highly recommended.
- For metal restorations, adhesive luting as well as conventional cementation can be used.
b) Translucency
To meet the increasing esthetic demands of the patients, new materials and techniques are continuously introduced, aiming to provide the perfect esthetic restorations. This includes not only new restorative materials but also new modifications to the luting agents as well. Highly translucent ceramics can deliver superior esthetics and therefore their popularity and clinical applications expanded widely among clinicians. It is nevertheless very important for the clinician to apprehend that the final esthetic result is influenced by the complete restorative complex and not just by the restorative material, as the luting agent is a key factor in achieving the desired high esthetics (21-24).
For that reason, the choice of an opaque conventional cement for cementation of high-translucent restoration should not be recommended as it can negatively influence the final esthetic results. Therefore, composite resin cements are the material of choice, as they are available in different shades and translucencies for the clinician to be able to choose the suitable resin cement to achieve the desired esthetics based on the restorative material and thickness as well as the color of the underlying abutment. Some composite resin cements offer try-in paste so that the clinician and the patient can visualize the final results before luting and therefore better choose the appropriate shade of the resin cement.
Conclusion / Clinical Significance:
- For all translucent ceramic restorations, adhesive luting is highly recommended.
- For metal and opaque high-strength zirconia restorations, adhesive luting as well as conventional cementation can be used.
3) SIMPLICITY OF THE WORKFLOW AND SPECIAL REQUIREMENTS OF THE WORKING ENVIRONMENT
The process of adhesive luting with full-adhesive composite resin cements (e.g. PANAVIA™ V5, Kuraray Noritake Dental Inc.) requires separate etching and priming procedures usually using a self-etch adhesive system (e.g. PANAVIA™ V5 Tooth Primer, Kuraray Noritake Dental Inc.) as well as a primer for the restorative material such as a universal primer that can be used for different substrates including metal, ceramics and composites (e.g. CLEARFIL™ CERAMIC PRIMER PLUS, Kuraray Noritake Dental Inc.). These procedures are technique sensitive and intolerant to contaminations, therefore the luting process needs a dry oral environment avoiding any contamination, such as saliva or blood, preferably using rubber dam, as any contamination can compromise the bond strength. Therefore, inability to maintain dry field as in case of subgingival preparation margins is considered a contraindication for traditional full-adhesive luting. However, this method provides very durable bond strength, therefore it is the luting method of choice for minimal invasive non-retentive preparations, such as resin-bonded FDPs, labial and occlusal veneers and inlay-retained FDPs, in which the retention is mainly dependent on the adhesion (9-11).
Still, in everyday practice, clinicians seek efficiency and effectivity by using a simple but durable luting agent for the insertion of full-coverage restorations such as tooth-or implant-supported crowns and FDPs. Although the conventional cements are simple and fast in their use, they provide little or no adhesion at all and therefore they are not recommended in several cases (6, 9, 14, 15, 19, 20). A simple but reliable method can be well accomplished by the use of self-adhesive resin cements (e.g. PANAVIA™ SA Cement Universal, Kuraray Noritake Dental Inc.) as they can be considered the best alternative for full-adhesive adhesive luting in less critical situations that do not rely entirely on adhesion (9, 15). Furthermore, self-adhesive resin cements are not as technique sensitive and intolerant to contaminations as traditional full-adhesive resin cements.
Typically, a MDP phosphate monomer is integrated in the self-adhesive resin cement, which is required to chemically bond to different substrates, making it possible for the resin cement to chemically bond to non-precious metals and zirconia as well as tooth substance. However, regardless of the self-adhesive resin cement, the use of a separate silane coupling agent is still required when bonding to silica-based ceramics (e.g. leucite, lithium silicate and lithium disilicate), hybrid ceramics and composite restorations.
Recently, a unique self-adhesive resin cement (PANAVIA™ SA Cement Universal, Kuraray Noritake Dental Inc.) was introduced: through an innovative and distinctive production technology, a silane-coupling agent (long carbon chain silane (LCSi)) is integrated in the cement, and thus being the real universal adhesive system that completely eliminate the need for any other adhesive or primer when being used for all substrates including glass ceramics. So the luting process can be in this case truly shortened to one step.
Therefore, this unique cement combines several advantages of adhesive luting as well as the straightforward procedure of the conventional cementation without compromising the clinical success, regardless of the type of the restorative material.
As a conclusion, adhesive luting has more benefits over conventional cementation, regarding retention, esthetics, stabilization of the tooth and the restoration as well as preventing micro leakage (6, 9, 14-17, 19, 20, 25, 26) (Table 1). Moreover, there are no absolute contraindications for adhesive luting other than hypersensitivity to methacrylate monomers, as self-adhesive resin cements can be used in cases where full-adhesive resin cements are contraindicated, such as inability to avoid contamination (Table 2). As a result, adhesive luting can be generally used in every clinical situation, whereas conventional cementation is limited (Table 3).
Dentist(s):
Prof. Dr. Florian Beuer
Professor and Chair, Department of Prosthodontics, Geriatric Dentistry and Craniomandibular Disorders, Charité – Universitätsmedizin Berlin, Germany.
Dr. Adham Elsayed
Clinical and Scientific manager, Kuraray Europe GmbH, Hattersheim, Germany.
References
1. Ladha K, Verma M. Conventional and contemporary luting cements: an overview. J Indian Prosthodont Soc. 2010;10(2):79-88.
2. Schwartz NL, Whitsett LD, Berry TG, Stewart JL. Unserviceable crowns and fixed partial dentures: life-span and causes for loss of serviceability. J Am Dent Assoc. 1970;81(6):1395-401.
3. Gilboe DB, Teteruck WR. Fundamentals of extracoronal tooth preparation. Part I. Retention and resistance form. J Prosthet Dent. 1974;32(6):651-6.
4. Muruppel AM, Thomas J, Saratchandran S, Nair D, Gladstone S, Rajeev MM. Assessment of Retention and Resistance Form of Tooth Preparations for All Ceramic Restorations using Digital Imaging Technique. J Contemp Dent Pract. 2018;19(2):143-9.
5. Edelhoff D, Özcan M. To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: cementation. Clin Oral Implants Res. 2007;18 Suppl 3:193-204.
6. Güth JF, Stawarczyk B, Edelhoff D, Liebermann A. Zirconia and its novel compositions: What do clinicians need to know? Quintessence Int. 2019;50(7):512-20.
7. Smith CT, Gary JJ, Conkin JE, Franks HL. Effective taper criterion for the full veneer crown preparation in preclinical prosthodontics. J Prosthodont. 1999;8(3):196-200.
8. Uy JN, Neo JC, Chan SH. The effect of tooth and foundation restoration heights on the load fatigue performance of cast crowns. J Prosthet Dent. 2010;104(5):318-24.
9. Blatz MB, Vonderheide M, Conejo J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J Dent Res. 2018;97(2):132-9.
10. Chaar MS, Kern M. Five-year clinical outcome of posterior zirconia ceramic inlay-retained FDPs with a modified design. J Dent. 2015;43(12):1411-5.
11. Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017;65:51-5.
12. Guth JF, Wallbach J, Stimmelmayr M, Gernet W, Beuer F, Edelhoff D. Computer-aided evaluation of preparations for CAD/CAM-fabricated all-ceramic crowns. Clin Oral Investig. 2013;17(5):1389-95.
13. Nordlander J, Weir D, Stoffer W, Ochi S. The taper of clinical preparations for fixed prosthodontics. J Prosthet Dent. 1988;60(2):148-51.
14. Blatz MB. Long-term clinical success of all-ceramic posterior restorations. Quintessence Int. 2002;33(6):415-26.
15. Blatz MB, Phark JH, Ozer F, Mante FK, Saleh N, Bergler M, et al. In vitro comparative bond strength of contemporary self-adhesive resin cements to zirconium oxide ceramic with and without air-particle abrasion. Clin Oral Investig. 2010;14(2):187-92.
16. Kern M, Thompson VP, Beuer F, Edelhoff D, Frankenberger R, Kohal RJ, et al. All ceramics at a glance. 3rd English Edition ed: AG Keramik; 2017.
17. Attia A, Abdelaziz KM, Freitag S, Kern M. Fracture load of composite resin and feldspathic all-ceramic CAD/CAM crowns. J Prosthet Dent. 2006;95(2):117-23.
18. Borges GA, Caldas D, Taskonak B, Yan J, Sobrinho LC, de Oliveira WJ. Fracture loads of all-ceramic crowns under wet and dry fatigue conditions. J Prosthodont. 2009;18(8):649-55.
19. Campos F, Valandro LF, Feitosa SA, Kleverlaan CJ, Feilzer AJ, de Jager N, et al. Adhesive Cementation Promotes Higher Fatigue Resistance to Zirconia Crowns. Oper Dent. 2017;42(2):215-24.
20. Weigl P, Sander A, Wu Y, Felber R, Lauer HC, Rosentritt M. In-vitro performance and fracture strength of thin monolithic zirconia crowns. J Adv Prosthodont. 2018;10(2):79-84.
21. Calgaro PA, Furuse AY, Correr GM, Ornaghi BP, Gonzaga CC. Post-cementation colorimetric evaluation of the interaction between the thickness of ceramic veneers and the shade of resin cement. Am J Dent. 2014;27(4):191-4.
22. Chang J, Da Silva JD, Sakai M, Kristiansen J, Ishikawa-Nagai S. The optical effect of composite luting cement on all ceramic crowns. J Dent. 2009;37(12):937-43.
23. Turgut S, Bagis B. Effect of resin cement and ceramic thickness on final color of laminate veneers: an in vitro study. J Prosthet Dent. 2013;109(3):179-86.
24. Volpato CA, Monteiro S, Jr., de Andrada MC, Fredel MC, Petter CO. Optical influence of the type of illuminant, substrates and thickness of ceramic materials. Dent Mater. 2009;25(1):87-93.
25. Al-Makramani BMA, Razak AAA, Abu-Hassan MI. Evaluation of load at fracture of Procera AllCeram copings using different luting cements. J Prosthodont. 2008;17(2):120-4.
26. Gu XH, Kern M. Marginal discrepancies and leakage of all-ceramic crowns: influence of luting agents and aging conditions. Int J Prosthodont. 2003;16(2):109-16.
Case by Max Andrup
The maxillary right first premolar of this patient had a huge defect on the lingual aspect extending subgingivally. In order to facilitate proper working field isolation for the placement of an onlay, it was decided to elevate the margin using the deep margin elevation (DME) technique. Moisture control is more easily handled with a matrix and composite compared to trying to keep a deep box dry at the placement of an indirect restoration. The preferred method used to maximize the bond strength to dentin was immediate dentin sealing combined with resin coating, while the luting material of choice was warmed light-curing resin composite (CLEARFIL™ AP-X). It shows a superior performance compared to dual-cure luting materials e.g. in terms of conversion of monomers to polymers, time available for excess removal, bio-mechanical properties and polymerization shrinkage stress.
Fig. 1. Pre-operative situaton with clearly visible deep distal margin. In reality, it was even deeper than the picture reveals. The Brinker Rubber Dam Clamp B4 placed here is a life saver in cases with subgingival margins. The buccal wall was still intact. We planned to reduce it to allow the onlay to cover it completely, allowing it to work under compression and thus increasing the fracture resistance.
Fig. 2. Situation after placement of a sectional matrix on thedistal aspect of the tooth. In order to retract the rubber dam mesially, PTFE tape was placed in this area. This allowed me to seal the dentin in a perfectly dry environment. For immediate dentin sealing, the smear layer developed on the dentin immediately after tooth preparation was compacted with the aid of air abrasion (50 μm alumina particles) to provide for the best possible bonding conditions, followed by the application of the bonding agent (CLEARFIL™ SE Protect). Afterwards, the bonded dentin was covered with a thin layer of flowable resin composite (CLEARFIL MAJESTY™ ES Flow). This resin coating ensures that the hybrid layer is thick enough and that the dentin is perfectly sealed.
Fig. 3. After immediate dentin sealing and resin coating. The hybrid layer was left to mature for approximately five minutes. This measure leads to an increased bond strength to dentin, which prevents issues that might occur due to the polymerization shrinkage stress occurring after composite placement. Subsequently, CLEARFIL™ AP-X was applied in small increments, starting in the distal box. In this way, the biobase was built up to the desired height. The main arguments for using CLEARFIL™ AP-X as a replacement for deep dentin are that the modulus of elasticity is within the same range as that of dentin and it exhibits an extraordinarily low polymerization shrinkage.
Fig. 4. Lateral view of the tooth at the day of delivery. View of the tooth at the day of delivery after rubber dam placement and prior to air-abrasion treatment of the biobase, which was performed to remove any remaining temporary cement. Following try-in, the lithium disilicate onlay was cleaned with KATANA™ Cleaner and pretreated with CLEARFIL™ Ceramic Primer. The biobase was sandblasted again for cleaning.
Fig. 5. Onlay in place after selective etching of the enamel with 35 % phosphoric acid etchant, and application of CLEARFIL™ SE Bond to the biobase and the intaglio of the onlay as well as luting with heated CLEARFIL™ AP-X. Excess composite was removed and the composite light cured.
FINAL SITUATION
Fig. 6. Occlusial view of the luted restoration.
Dentist:
Max Andrup graduated from the University of Umeå in 2010 and today runs his private practice in the city of Hudiksvall, Sweden. He has a passion for restorative dentistry with a biomimetic approach.
Clinical case with CLEARFIL™ MAJESTY ES-2 Universal
Case by Dr Paul Guicherit
A girl presented to the dental office after a bicycle accident. She had a traumatized maxillary left central incisor and an abrasion injury was visible on and above her upper lip.
The tooth was restored immediately using CLEARFIL™ MAJESTY ES-2 Universal in the shade UL (Universal Light).
The outcome was excellent due to a great optical integration and an invisible transition between the tooth and the resin composite.
Clinical photo credits: Dr Paul Guicherit
Case by Max Andrup
This is the story of cusp fracture due to cuspal tension. This is a common weakness of amalgam-restored teeth associated with expansion of the restorative material. The affected maxillary right first premolar was restored with a crownlay.
For seating of the crownlay, the use of warmed light-curing resin composite (CLEARFIL™ AP-X) has proven its worth. Compared to a dual-cure luting resin, the selected material offers many benefits including the fact that the heat assists in the conversion of monomers to polymers, the time available to remove excess is almost unlimited, and the composite offers better bio-mechanical properties as well as a lower polymerization shrinkage stress.
Fig. 1. Pre-operative situation. The patient requested for an emergency appointment, where we temporarily fixed the lost buccal cusp and made a new appointment for a crownlay preparation. After removing the amalgam and temporary filling, the remaining amount of tooth structure was quite beneficial with a large lingual cusp and a ring of enamel around the whole tooth.
Fig. 2. The decision was made to reduce the lingual cusp and to place a crownlay working in compression. As the thickness of the cusp was adequate for an onlay, this treatment option would have been equally suitable. After tooth preparation, immediate dentin sealing was performed: For this purpose, I air-abraded the dentin to remove the smear layer and give the adhesive the best condition for a strong bond to dentin. Then, CLEARFIL™ SE Protect was applied to the tooth surface and covered with a thin layer of flowable resin composite (CLEARFIL MAJESTY™ Flow) to ensure a total seal.
Fig. 3. The resin composite surface was air-abraded with 50 μm zirconia particles, followed by selective etching of the enamel with a 35-percent phosphoric acid etchant. After try-in of the crownlay made of lithium disilicate, the tooth surface and the restoration were cleaned with KATANA™ Cleaner.
FINAL SITUATION
Fig. 4. The cleaned crownlay was pre-treated with CLEARFIL™ Ceramic Primer, before warmed CLEARFIL™ AP-X was applied to both tooth structure and restoration for luting. The colour of the crownlay matched the colour of the adjacent premolar, while the visible part of the restored tooth’s remaining structure was stained from amalgam corrosion.
Dentist:
Max Andrup graduated from the University of Umeå in 2010 and today runs his private practice in the city of Hudiksvall, Sweden. He has a passion for restorative dentistry with a biomimetic approach.
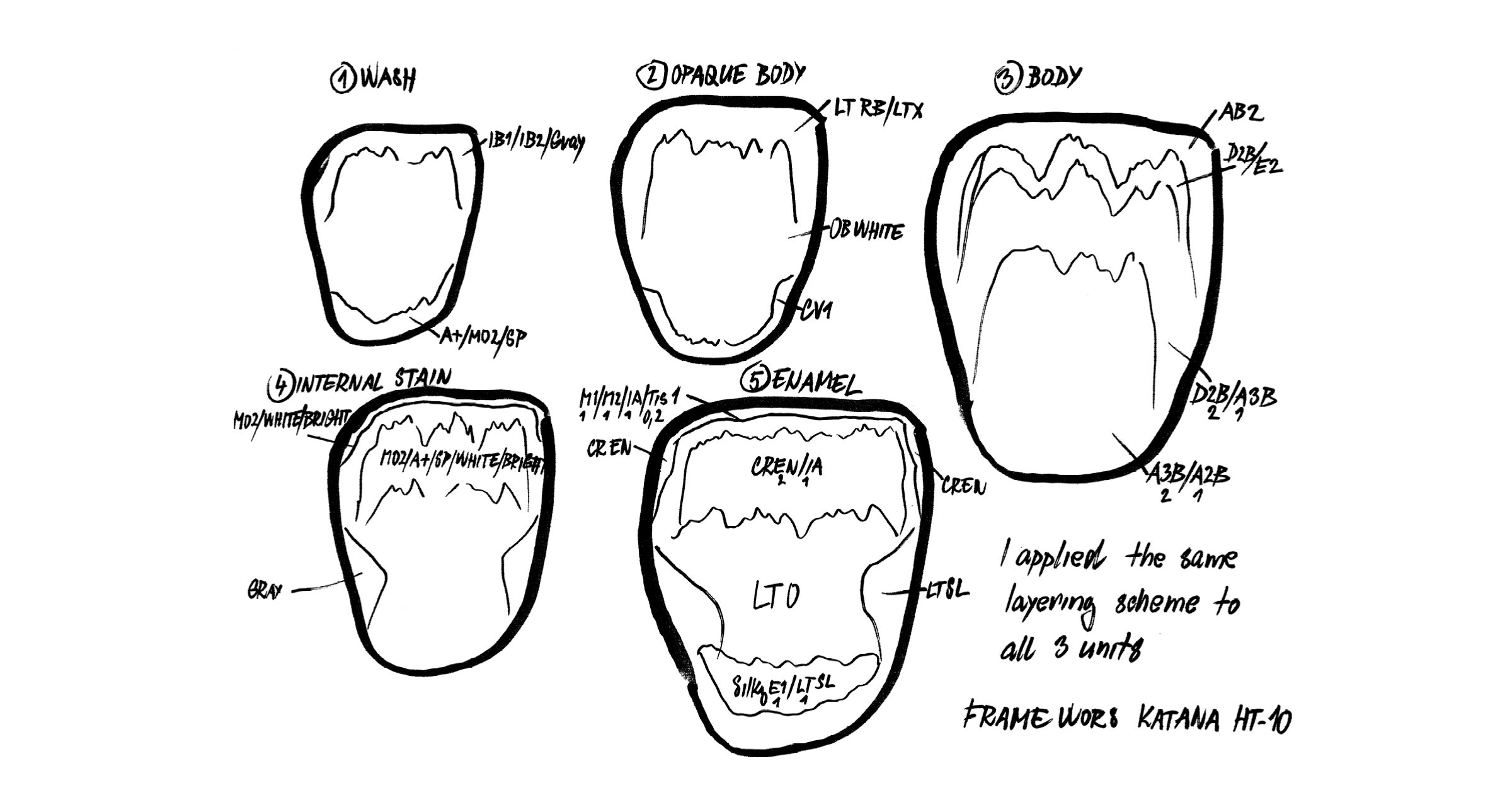
Clinical case - Crowns on 12/11/21/22
By Dr Alessandro Devigus
This video illustrates the Cementation of Katana STML Crowns with Panavia V5.
Dentist:
DR. ALESSANDRO DEVIGUS
Dr. Alessandro Devigus received his degree from Zurich University, Switzerland, in 1987. Since 1990 his working in his own private practice with a focus on CAD CAM and Digital Dentistry. He is also CEREC Instructor at the Zurich Dental School.
Dr. Alessandro Devigus is an active member of the European Academy of Esthetic Dentistry (EAED), founder of the Swiss Society of Computerized Dentistry, Neue Gruppe member, ITI fellow and speaker.
Dr. Devigus is editor-in-chief of the International Journal of Esthetic Dentistry, author of various publications and an international lecturer.
Case by Max Andrup
This patient had requested for an emergency appointment and presented with severe erosive tooth wear in several teeth, a crack in the mesial wall of the maxillary first molar and a failing direct restoration with recurrent decay on the adjacent second premolar. I decided to replace the direct resin composite restoration immediately as this was the main cause of discomfort. It was decided to restore the other defects during the next appointment.
The resin composite of choice was CLEARFIL MAJESTY™ ES-2 (Universal shade concept), an innovative material with a single universal shade designed for posterior restorations. The manufacturer claims that, due to the integration of Kuraray Noritake Dental Inc.’s light diffusion technology, this universal shade nicely blends in with the surrounding tooth structure virtually independent of its colour. Curious about the real potential of this concept, I wanted to put the material to a test.
Fig. 1. Pre-operative situation revealing signs of severe erosive tooth wear, a cracked mesial wall of the first molar and a failed filling on the second premolar with recurrent decay.
Fig. 2. Appearance of the tooth after removal of the direct composite restoration. The recurrent caries is obvious.
Fig. 3. Caries Detector applied to the decayed tooth structure.
Fig. 4. Establishing of a peripheral zone totally free of caries with the aid of Caries Detector. It may be useful to apply the dye several times.
Fig. 5. The final situation after several applications of Caries Detector. The peripheral zone is completely free of caries, which is a strict requirement for the establishment of a perfect seal during bonding. Affected caries stained light pink is not removed not to risk going near the pulp.
Fig. 6. Build-up of the proximal wall with CLEARFIL MAJESTY™ ES-2 (U shade) after the application of CLEARFIL™ SE Protect and a small layer of CLEARFIL MAJESTY™ ES Flow in a thickness of about 0,5 mm. By focusing on the proximal wall connecting to enamel first, the hybrid layer is given the time needed to mature. Not putting a new increment on top of the hybrid layer for the first five minutes will lead to an increased bond strength to dentin.
FINAL SITUATION
Fig. 7. Appearance of the tooth immediately after finishing and polishing. Although the rubber dam is still in place and the tooth structure is not yet rehydrated, it is evident that the composite blends in very well with the remaining tooth structure to form a seamless margin.
Dentist:
Max Andrup graduated from the University of Umeå in 2010 and today runs his private practice in the city of Hudiksvall, Sweden. He has a passion for restorative dentistry with a biomimetic approach.
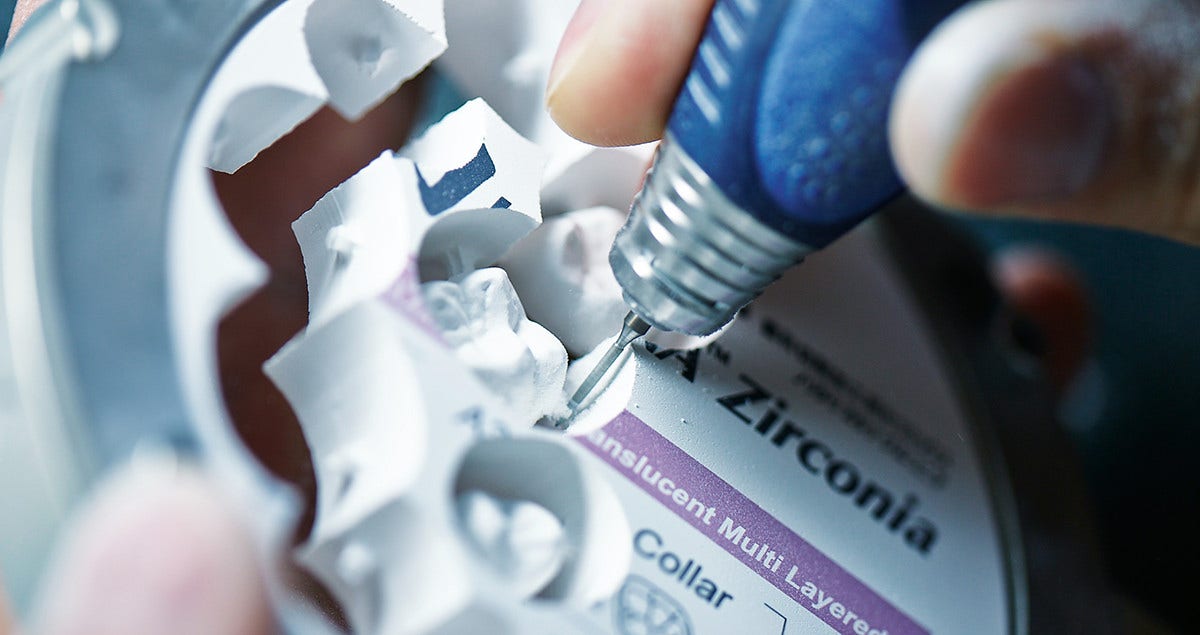
ZIRCONIA IN DENTISTRY
Zirconia ceramics are increasingly being used for dental prostheses. In the past, they were used as a substructure that was baked with porcelain; nowadays, monolithic zirconia prostheses have been made possible by the introduction of aesthetic zirconia ceramics varieties. They are used more and more, even as RBFDPs (Resin Bonded Fixed Dental Prosthesis).
There is currently quite a lot of discussion about zirconia. So much the better, because it keeps the dynamics of the subject alive. Is it possible to adhesively cement zirconia? Is it permissible to sandblast zirconia? Is it feasible to polish zirconia? Is wear of the antagonist an issue? And so on and so forth.
New dental technologies and materials have been developed in recent years to meet the demand for aesthetic, biocompatible and metal-free prostheses. Although porcelain has been used as an aesthetic dental material for more than hundred years, its restrictions are now well-known. It is the fragility of porcelain (low flexural strength and fracture toughness) in particular which restricts its application in areas where the exertion of massive force on the material is a factor. Zirconia has a high flexural strength and is therefore suitable for multiple dental applications.
Development
The first generation of zirconias used in dentistry belonged to the Partially Stabilised Zirconia (PSZ) class. This type of zirconia, stabilised with yttrium oxide, was composed of a mix of monoclinic, tetragonal and cubic crystals but is no longer used nowadays. The so-called Y-TZP variant was then used for many years, and still is. Its main characteristics are high flexural strength (> 1.000 MPa) and an opaque white appearance. For the most part, this variant is composed of tetragonal crystals of a few hundred nanometers. To keep the material stable at room temperature, approximately 3 mol% of yttrium oxide is added to the composition, which is why it is sometimes referred to as 3Y zirconia.
In order to improve its aesthetic properties, a start was made on the development of a new variety, so-called cubic zirconia. Cubic zirconia is characterised by a high translucence, meaning that a lower flexural strength must be accepted. Admittedly, the flexural strength of this variant is lower than that of the tetragonal variety, but still much higher than the flexural strength of lithium disilicate. It also contains more yttrium oxide; approximately 5 mol%.
Crystal phases
We currently know zirconia crystals in three varieties: monoclinic, tetragonal and cubic. In general, zirconia only exists in the monoclinic phase at room temperature. Monoclinic zirconia has low strength as well as low translucence. Tetragonal zirconia crystals are metastable and can only exist at room temperature after having been stabilised with yttrium oxide, among other metal oxides. The characteristics of tetragonal zirconia are that it is strong, but at the same time devoid of aesthetic
properties. Cubic crystals are stable and ensure improved translucence. Although prostheses made from cubic zirconia are not as strong as the tetragonal variety, they are highly aesthetic, and are even suitable for monolithic restorations in the aesthetic zones.
Multilayer
KATANA™ Zirconia ML, STML and UTML, as well as the latest KATANA™ Zirconia Block, are so-called multilayer zirconias. These products are built up of four layers with an ascending degree of translucency, ranging from the more opaque and coloured body layer (cervical), through two transitional layers, to the translucent incisal edge (occlusal/incisal). The invisible transition from one layer to another is achieved using a unique process. The secret is in the specific distribution of particles during the pre-sintered stage (continuous gap grading). In combination with the cold isostatic pressing method, this ensures material of an outstandingly high quality.
KATANA™ Zirconia Block
The use of KATANA™ Zirconia Block makes it possible to produce a complete monolithic zirconia prosthesis in a short time. This block was developed to be used within the CEREC workflow. After scanning, the prosthesis is ground for approximately 15 minutes and can then be sintered in the SpeedFire oven in just half an hour1). KATANA™ Zirconia Block shares the properties of KATANA™ STML and can be used for the production of single-unit prostheses such as full crowns for both anterior and posterior applications.
Wear of the antagonist
The question of whether zirconia prostheses are harmful to the antagonist would seem to be justified; after all, this is a very hard material. Hardness, however, does not relate directly to the abrasive properties of a material. Smoothly polished zirconia is minimally abrasive, something which has been corroborated by multiple studies2). Glaze, porcelain, lithium disilicate and even enamel are all more abrasive for the antagonist.
CAD/CAM
Thanks to emerging digital solutions (CAD/CAM) combined with the possibility of executing fixed partial dentures (FPDs) in monolithic zirconia, a fully digital workflow - from scan to prosthesis - is now feasible.
Sandblasting
Sandblasting using alumina is the standard method for the roughening of zirconia. In order to reduce the decline from the tetragonal crystal stage to the monoclinic stage, it is recommended that sandblasting be carried out at a maximum pressure of 2.5 bar using 50 micron aluminium oxide particles as a maximum3). In practice, zirconia is also frequently sandblasted tribochemically, for example, by means of CoJet (3M). The results achieved with this method are variable. In the case of limited pressure (2.5 bar as a maximum) there is a risk that the energy will be insufficient to achieve an effective and complete fusion between the silica and the zirconia surface. It is therefore recommended that CLEARFIL™ Ceramic Primer Plus be used for adhesive connection with the sandblasted surface. The silane in this ceramic primer bonds chemically with the silica, while the MDP bonds with the areas of zirconia not covered by silica. The use of silane alone does not provide an adequate basis for a reliable result4). Sandblasting with alumina, however, followed by priming with CLEARFIL™ Ceramic Primer Plus, is a well-proven and reliable method to ensure effective bonding to zirconia5).
Not etchable, but certainly bondable
Zirconia is not – or is barely – etchable with the etching technology available (HF). In addition, it cannot be recommended that zirconia be treated with phosphoric acid, because of the bonding of phosphates to the surface of the zirconia, which will inhibit a chemical activation of the surface for some adhesive cementation systems. The question of whether an etching product should be used is a valid one; after all, chemical etching is not necessary to achieve surface roughness. Achieving surface roughness is, however, a logical option, and roughening by means of sandblasting would seem to be the most appropriate method for zirconia. Thereafter, chemical bonding is ensured using a phosphoric functional monomer, preferably MDP.
Adhesion principles
Three basic factors are required to achieve the effective bonding of different materials. In keeping with the principles of adhesion, these are: surface enlargement (micromechanical retention), chemical activity (adsorption and electrostatic bonding) and a high-energetic surface to guarantee proper adaptation.
Adhesive bonding
The best method of adhesive bonding for zirconia is the use of a composite cement containing MDP. Professor Mathias Kern published an article about bonding to zirconia using MDP as early as 1998. This study showed that sustainable resin bonding to zirconia can only be achieved using a composite cement with a special adhesive monomer. The monomer used was in fact MDP. In the meantime, many studies have been published about bonding to zirconia.
On the one hand, these studies concern bonding with phosphate monomers (MDP); on the other hand, attention has been paid to the modification of the zirconia surface to render it etchable. The simplest and most reliable method is to sandblast the surface at a low pressure using aluminium oxide, followed by priming with an MDP-containing primer6).
PETER SCHOUTEN,
Technical Manager Kuraray Europe Benelux
1) Depending on the method of grinding/milling.
2) Mörmann W.H. et al. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: Two body wear, gloss retention, roughness and Martens hardness. Journal of the mech. Behavior of Biomedical Materials 20 (2013) 113-125, Janyavula S. et al. The wear of polished and glazed zirconia against enamel. J Prosthet Dent 2013; 109;22-29 Stawarczyk B. et al. Comparison of four monolithic zirconia materials with conventional ones: Contrast ratio, grain size, four-point flexural strength and two-body wear. Journal of the mech. Behavior of Biomedical Materials 59 (2016) 128-138 D’Arcangelo C. et al. Wear Evaluation of Prosthetic Materials Opposing Themselves. Oper Dent 2017 antagonistic surface roughness on the wear of human enamel and nanofilled composite resin artificial teeth. J Prosthet dent 2009; 101: 342-349.
3) Attia A. / Kern M. Effect of cleaning methods after reduced-pressure Air Abrasion on Bonding to Zirconia Ceramic J Adhes Dent 2011; 13: 561-567.
4) Pilo R. Effect of tribochemical treatments and silane reactivity on resin bonding to zirconia. Dent Mater (2017).
5) Kern M. Bonding to oxide ceramics - Laboratory testing versus clinical outcomes. Dent Mater (2014).
6) M. Kern et al., Bonding to zirconia ceramic: adhesion methods and their durability. Dent Mater 14: 64-71, Jan.1998.
Effectiveness of temporary cement removal
Did you know that a complete removal of temporary cement from the abutment tooth with a rubber cup and pumice paste or an ultrasonic scaler is usually impossible? In most cases, some visibly undetectable residues remain on the surface. They will negatively affect the bonding performance of the permanent cementation system you selected. KATANA™ Cleaner is our answer to this problem! Applied after conventional temporary cement removal, it provides optimal conditions for permanent cementation.
All relevant details are revealed in this scientific report.
By Aleksandra Łyżwińska, DMD
The MOD restoration on the maxillary left second premolar of this patient was in need of replacement. It was decided to create a direct composite overlay with CLEARFIL MAJESTY™ ES Flow - Super Low A3, CLEARFIL MAJESTY™ ES-2 Classic A2. CLEARFIL™ SE BOND 2 was used after selective etching of the enamel to establish a chemical bond to enamel and dentin. For the finishing and polishing procedure, abrasive discs were used first, followed by silicon carbide rubber instruments and the CLEARFIL™ Twist DIA system.
Fig. 1. Initial clinical situation revealing the composite restoration to be replaced on the second premolar.
Fig. 2. Occlusal view of the teeth after cavity preparation including cusp reduction.
Fig. 3. Lateral view of the teeth after cavity preparation.
Fig. 4. Matrix band held in place with wedges and two rings.
Fig. 5. Situation after etching, bonding, removal of one ring, and build-up of the interproximal walls with CLEARFIL MAJESTY™ ES-2 Classic in the shade A2.
Fig. 6. Cavity filled with CLEARFIL MAJESTY™ ES Flow - Super Low A3.
Fig. 7. Occlusal surface restored with CLEARFIL MAJESTY™ ES-2 Classic in the shade A2.
Fig. 8. Polishing with the pre-polisher of the CLEARFIL™ Twist DIA system.
Fig. 9. Polishing with the high-shine polisher of the CLEARFIL™ Twist DIA system.
Fig. 10. Appearance of the restoration immediately after rubber dam removal and checking of the occlusal contacts.
FINAL SITUATION
Fig. 11. Linguo-occlusal view of the treatment outcome.
Fig. 12. Lateral view of the treatment outcome.
Dentist:
ALEKSANDRA ŁYŻWIŃSKA
Warsaw, Poland
Aleksandra Łyżwińska, DMD, is a passionate aesthetic and adhesive dentist. Driven by Evidence Based Dentistry, her goal includes using modern composite materials and bonding agents in her clinical practise. In addition to her primary job, she worked as a lecturer and an assistant professor at the Department of Conservative Dentistry and Endodontics of Medical University of Warsaw, her alma mater.