Case by Dr. Hendrik Zellerhoff
Not all zirconia is created equal. This finding presented by Prof. Martin Rosentritt7 back in 2014 has lost none of its actuality and even appears to be increasingly relevant these days. This is because dental practitioners are spoilt for choice between various zirconia blanks, which differ widely in terms of quality, flexural strength, shade appearance, translucency and production complexity. Hence, each material has its own specific processing requirements and range of indications6. Profound knowledge of the available zirconia options is therefore an absolute prerequisite for long-term success of every full contour restoration produced in a time-efficient and economic procedure.
While in the early years of zirconia manufacturing in dentistry, the dental practitioner’s choice was limited to industrially milled zirconia frameworks hand-veneered by the dental technician, a wide range of material variants for chairside CAD/CAM production is nowadays available. Material-specific improvements are one of the reasons for the fact that every single zirconia has its specific indications and its own material parameters6. Zirconia milling blocks for monolithic restorations are in principle very well suited for the chairside production of single crowns for the anterior and specifically the load bearing posterior area. This is due to their stability and the reduced processing effort compared to hand- veneered crowns. However, the material in use needs to fulfil high demands with regard to strength, translucency, and shading – parameters that also need to be balanced against each other2 (Fig. 1 to 4).
Fig. 1. Initial situation with multiple insufficient fillings.
Fig. 2. Crown milled from a KATANA™ Zirconia Block (Kuraray Noritake Dental Inc., Tokyo, Japan).
Fig. 3. Crown glazed after sintering, with fissures characterized using stains.
Fig. 4. Adhesively cemented crown with the appearance of a natural molar.
NOT ALL ZIRCONIA IS CREATED EQUAL
Due to their high flexural strength of more than 1,000 MPa, tetragonal zirconia variants (3Y-TZP) of the first and second generation are perfectly suited as framework materials. However, they lack the translucency required for monolithic use. It is theoretically possible to improve the translucency of 3Y-TZP materials by increasing the sintering temperature, however, this would result in restorations with insufficient strength. This is different for the third and fourth generations of cubic-tetragonal zirconia (5- TZP and 4-TZP). Due to the increased yttria content in the formulation, cubic crystals grow in the crystal microstructure. These cubic crystals have a larger volume, which leads to reduced scattering at the grain boundaries and improved light transmission. In addition, cubic crystal structures are more isotropic than tetragonal structures, so that incoming light is spread more evenly into all directions8. The combination of a high flexural strength and a high translucency in the fourth generation zirconia sets the stage for monolithic use of the material. This, in turn, eliminates the risk of chipping of the veneering porcelain.
PREMISES OF MONOLITHIC CHAIRSIDE RESTORATIONS
In order to ensure the desired long-term stability, intraoral functionality and aesthetics of a monolithic restoration on one hand and a time- and cost-efficient chairside workflow on the other, two factors are crucial. One is a proper functional occlusal adjustment of the restorations, the other is knowledge about the material parameters of the zirconia blocks in use.
Hardness and abrasion
Clinically, monolithic zirconia shows virtually no abrasion and an antagonist-friendly behaviour - provided that the occlusal surface is polished properly, is free of sharp edges and is covered with glaze. In order to leverage this effect and to avoid improper occlusal contacts as factors triggering parafunctions, the dental practitioner should carefully carry out an occlusal and functional analysis. This analysis should include an examination of the vertical dimension and of different jaw movement like protrusion, retrusion, laterotrusion and mediotrusion. Based on the results, a precise dynamic occlusal adjustment is possible. Any retrospective adjustment – even in case of minimal irregularities – is impossible or, more specifically, restricted to the glazing layer. If the surfaces, especially the cusps, are not polished to a high gloss, any wear of the glaze would lead to the exposure of a rough abrasive zirconia surface. Material-specific high-gloss polishing and glazing, however, effectively avoids abrasive wear of the antagonist3,4,5.
Strength, translucency and shade
Under these premises, 5Y-TZP materials like KATANA™ Zirconia UTML (Ultra Translucent Multi Layered) with a flexural strength of 557 MP and a translucency of 43 percent are particularly well suited for the production of highly aesthetic anterior crown or veneer restorations. In the load-bearing posterior area, however, higher flexural strength values are necessary. Using 4Y-TZP materials like KATANA™ Zirconia Block (Super Translucent Multi Layered) with a flexural strength of 763 MPa provides more stability of the restoration, which is required for the posterior region. The product offers a translucency of 38 percent and is suitable for the chairside production of aesthetically and functionally demanding restorations with high stability even in case of a reduced wall thickness. Thanks to the colour gradient, light shines through in the incisal area in an enamel-like way, while in the cervical area, the level of translucency is similar to dentin. The imitation of a colour gradient found in natural teeth, which ensures that the restoration will blend in perfectly with the adjacent teeth, is obtained with a multi-layered, polychromatic structure with a smooth shade transition from the incisal to the cervical part. This feature eliminates the need for a time-consuming manual application of shades prior to sintering. A patient- specific post-sintering characterisation with stains is optional. As shade, form and effects are already visible during application, the dental practitioner gains full control over aesthetics at all times (Fig. 5 to 8).
Fig. 5. Comparison of flexural strength and translucency.
Fig. 6. Smooth shade transition from the enamel to the dentin and cervical area.
Fig. 7. Comparison of the translucency exhibited by different ceramics.
Fig. 8. Range of shades of KATANA™ Zirconia Single Unit Blocks.
KATANA™ ZIRCONIA BLOCK IN THE CEREC WORKFLOW
Reliable material properties are imperative for a smooth production workflow leading to a consistent high quality of the restorations. They are only obtained with industrially produced zirconia blanks, which offer a defect-free, homogeneous grain structure1,10. At Kuraray Noritake Dental, the whole manufacturing process of zirconia products is carried out in-house, including the production of the raw materials. Therefore, it is possible to optimize the material parameters of KATANA™ Zirconia Blocks for chairside production and with high-speed sintering process. Using these components, the dental practitioner can reduce the time needed for the production of a monolithic zirconia restoration including scanning, milling and sintering to less than an hour.
Design
For this purpose, the teeth to be restored are prepared and captured together with the adjacent and antagonist teeth using an intraoral scanner (Omnicam or Primescan, Dentsply Sirona). The digital data set is then imported into the CEREC software. The software extracts the required information from the data and generates a design proposal for the restoration. Usually, this proposal may be accepted without major modifications. Due to the high mechanical properties of KATANA™ Zirconia, a wall thickness of 1.0 mm is sufficient for a posterior crown. This design has two positive effects: it optimizes the translucency of the restoration and supports a minimal preparation, which also facilitates clinical procedures in situations with limited space conditions. The shade and translucency of the restoration is also customizable via virtual positioning of the designed crown in the multi-layer block. This enables the dental practitioner to harmonize the brightness and translucency with the parameters of the adjacent teeth (Fig. 9 to 13).
Fig. 9. Initial situation with insufficient porcelain layer.
Fig. 10. Abutment teeth after preparation prior to digital impression taking.
Fig. 11. Restorations after polishing, occlusal and cervical characterization and glaze firing.
Fig. 12 - 13. Final restorations in place - occlusal and frontal view.
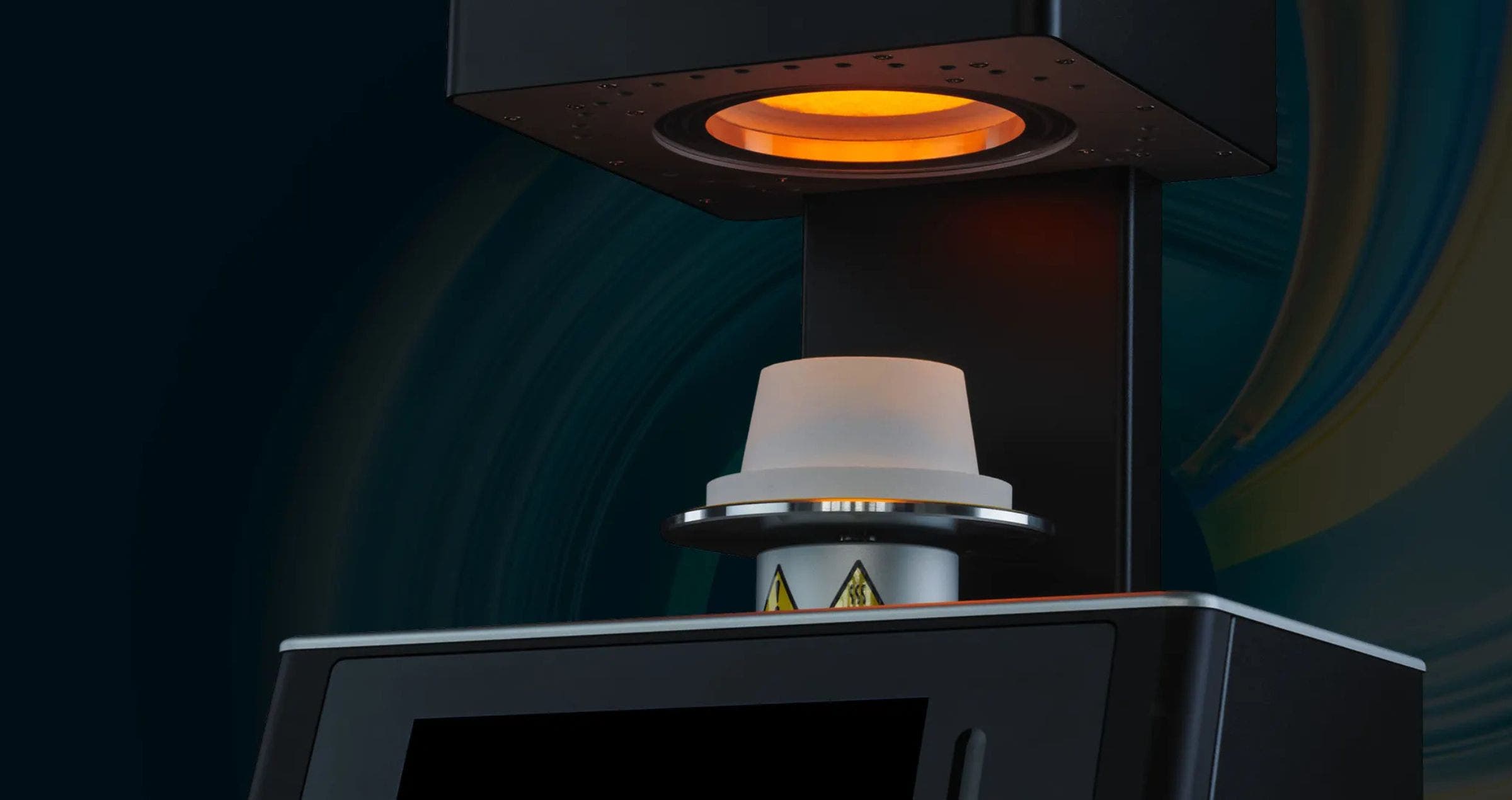
Sintering
The designed crown is milled from the KATANA™ Zirconia Block with the CEREC milling machine. Subsequently, finishing steps are carried out and the sintering process is started using the induction furnace CEREC SpeedFire. This furnace reaches a maximum heating rate of 300° C per minute. Neither pre-heating is required nor holding temperatures needed. As the material properties of KATANA™ Zirconia Block are optimally aligned with the CEREC SpeedFire programme, the user can be sure that the device adheres to all sintering parameters. This, in turn, is important for the growth of the crystals as well as phase transformation and stabilization9, which affect the natural shade results after sintering (Fig. 14 to 18).
Fig. 14 - 15. Labial and palatal view of the initial situation with restorations on the lateral incisor and canine.
Fig. 16. Varying shade and translucency gradient depending on the position of the restoration in the multi-layer block.
Fig. 17. Crowns with a natural colour gradient from the incisal to the cervical area merely glazed after sintering (without any additional adjustment).
Fig. 18. Natural aesthetic appearance of the KATANA™ Zirconia crowns even in the esthetic zone.
Individualisation and characterization
After sintering, dental practitioners may individualize or characterize KATANA™ Zirconia Block restorations if desired. This requires only a few simple work steps. The marginal ridges, mamelons, fissures or enamel cracks are imitated controllably using paste stains (CERABIEN™ ZR FC Paste Stain, Kuraray Noritake Dental), as the shade, shape and effects created are already visible during application. For the final glaze firing process with Glaze or Clear Glaze (Kuraray Noritake Dental), the SpeedFire induction furnace is used again (Fig. 19 to 25).
Fig. 19. Initial situation with secondary caries below the amalgam restoration on the maxillary left second premolar (tooth #25).
Fig. 20. Tooth prepared for a core build-up after caries excavation and proximal modification of the adjacent premolar (tooth #24).
Fig. 21. Crown milled from the block before …
Fig. 22. … and after sintering (at try-in).
Fig. 23. Fissures with age-specific characterization.
Fig. 24. Functional contact point created in consideration of the adjacent teeth.
Fig. 25. Final crown after glazing and adhesive cementation with PANAVIA™ V5 (Kuraray Noritake Dental).
Conditioning and placement of the restoration
Prior to restoration placement, the inner surface of the crown is sandblasted with Al2O3 (grain size: 50 μm, pressure: 1 bar) and treated with CLEARFIL™ Ceramic Primer Plus (Kuraray Noritake Dental), whereas PANAVIA™ V5 Tooth Primer (Kuraray Noritake Dental) is applied to the prepared tooth structure. Finally, PANAVIA™ V5 (Kuraray Noritake Dental) is applied for adhesive luting of the crown. The MDP monomer contained in the primer establishes a stable chemical bond and eliminates the need for additional conditioning. The fact that PANAVIA™ V5 is free of amines ensures long-term colour stability of the restoration.
CONCLUSION
With its combination of a high translucency and a high flexural strength, chairside dentists may use KATANA™ Zirconia Block for monolithic restorations with confidence. Restorations made of KATANA™ Zirconia offer the required long-term stability and fulfil the high aesthetic standards demanded from it to be able to serve as an alternative not only to cast metal and PFM crowns, but also to glass ceramic restorations. Due to the lack of a porcelain layer, the risk of chipping does not exist. Optimally aligned components enable dental practitioners to make use of a simplified and constantly monitored digital workflow that offers a high process reliability. Aesthetic functional restorations for the load-bearing posterior and the anterior area can be produced and placed within a single appointment. This is an important factor, which greatly affects patient satisfaction.
Dentist:
DR. HENDRIK ZELLERHOFF
References
1. Edelhoff D, Beuer F, Schweiger J, Brix O, Stimmelmayr M, Güth JF. CAD/CAM-generated high-density polymer restorations for the pretreatment of complex cases: a case report. Quintessence Int 2012;43:457–467.
2. Güth JF, Magne P. Optische Integration von CAD/CAM-Materialien. Int J Esthet Dent 2016;11:380–395.
3. Preis V, Behr M, Handel G, Schneider-Feyrer S, Hahnel S, Rosentritt M. Wear performance of dental ceramics after grinding and polishing treatments. J Mech Behav Biomed Mater 10 (2012); 13-22.
4. Preis V, Weiser F, Handel G, Rosentritt M. Wear performance of monolithic dental ceramics with different surface treatments. Quintessence Int 44 (2013);393-405.
5. Rosentritt M, Behr M, Strasser T, Preis V. Zirkonoxide als Implantatwerkstoff? Quintessenz 2018; 69 (12): 1420–1430.
6. Rosentritt M, Kieschnick A, Hahnel S, Stawarczyk B. Werkstoffkunde-Kompendium. Zirkonoxid. Berlin: Apple ibook; 2018.
7. Rosentritt M. Studie zum Verschleißverhalten von Zirkonoxid – Zirkonoxid ist nicht gleich Zirkonoxid. ZWR 2014;123(11):570-571.
8. Stawarczyk B, Keul C, Eichberger M, Figge D, Edelhoff D, Lümkemann N. Werkstoffkunde-Update: Zirkonoxid und seine Generationen – von verblendet bis monolithisch. Quintessenz Zahntech 2016;42(6):740–765.
9. Stawarczyk B, Özcan M, Hallmann L et al. The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clin Oral Investig 2013; 269–274.
10. Stober T, Bermejo JL, Rammelsberg P, Schmitter M. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehabil 2014;41:314–322.