Article by Dr. Adham Elsayed
High-performance adhesive resin cements are often the enablers of minimally invasive prosthodontic treatments. When the main aim is to save as much healthy tooth structure as possible, preparation designs that offer sufficient macro-mechanical retention for conventional cements are usually abandoned. The designs chosen instead need to rely on a strong and durable chemical adhesion established between the tooth structure and the restorative material – a task successfully accomplished by modern adhesive resin cement systems.
An excellent example of a minimally invasive, non-retentive preparation and restoration design is the single-retainer resin-bonded fixed dental prosthesis (RBFDPs), nowadays usually made of 3Y-TZP zirconia. With its single cantilever bonded to the oral and proximal enamel surface of an adjacent tooth, it requires minimal to no healthy tooth structure removal. The RBFDP is often used to replace a congenitally missing tooth – in many cases a maxillary lateral incisor – in young patients with incomplete dentoalveolar development and narrow edentulous spaces unsuitable for conventional implant placement1 (Fig. 1 and 2). Additional factors hindering implant therapy – like an insufficient bone volume or angulated roots – are also not an issue for this type of restoration. And compared to orthodontic gap closure, the treatment approach with a RBFDP is less risky, as it does not affect the vertical jaw relationship, prevent canine guidance or compromise the aesthetic appearance2. Finally, it is much less invasive than conventional FDPs, which is usually not a treatment option for young patients in the anterior region. The level of patient satisfaction and the success rates of this treatment approach are impressive3-7.
Fig. 1-2. Replacement of both congenitally missing maxillary lateral incisors with single-retainer zirconia RBFDPs after soft tissue augmentation and gingival margin correction.
Despite the numerous advantages and excellent clinical performance – single-retainer RBFDP made of zirconia showed a survival of 98.2 percent and a success rate of 92.0 percent after ten years4 – many dental practitioners still opt for alternative treatment options. The reason may be a lack of trust in the bond strength and durability to zirconia. However, this bond can be very strong and durable – provided that a few rules are respected.
HOW TO ESTABLISH A STRONG BOND TO THE TOOTH STRUCTURE
In order to decide whether a missing tooth may be successfully replaced by a single-retainer RBFDP made of zirconia, the abutment tooth should be examined carefully. It needs to be vital and largely free of caries or direct restorations, while the oral enamel surface must be large enough for resin bonding1. In addition, the space required for the placement of a retainer wing (thickness: about 0.7 mm) needs to be available, as a non-contact design is important for the success of the restoration. Among the preparation designs described in the literature is a lingual veneer and small proximal box preparation with retentive elements located in the enamel only1, or no preparation at all7. For restoration placement, the abutment tooth is treated as usual: after cleaning e.g., with fluoride-free prophylaxis paste, phosphoric acid etchant is applied to the bonding surface, which is then thoroughly rinsed and dried.
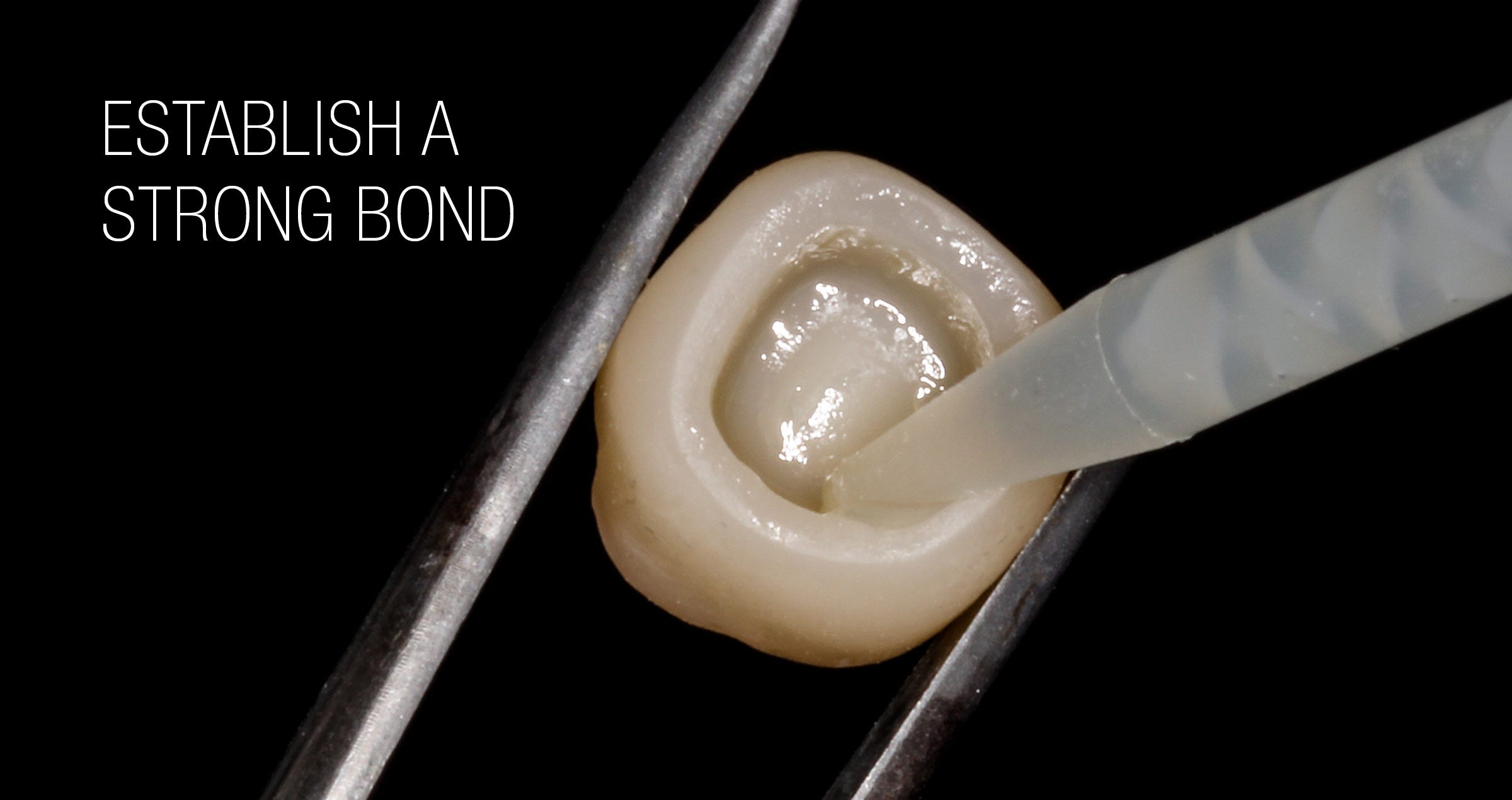
HOW TO ESTABLISH A STRONG BOND TO THE RESTORATION
The recommended pre-treatment for the bonding surface of the retainer wing made of zirconia is small-particle (50 μm) aluminium oxide air-abrasion at a low pressure (approx. 1 bar)8,9, followed by ultrasonic cleaning. Figures 3 (A-E) shows the sequence of surface treatment of zirconia restorations. As a visual aid for a controlled air-abrasion treatment, the marking of the surface with a pen has proven its worth. The whole air-abrasion procedure should be carried out after try-in, during which the tooth surface and the restoration usually becomes contaminated through contact with saliva and sometimes blood. Proteins present in saliva and blood that contaminate the bonding surface are safely removed in this way, while the required surface modification necessary to establish a strong and durable bond to the selected resin cement system is achieved10.
FIGURE 3: SEQUENCE OF SURFACE TREATMENT OF ZIRCONIA RESTORATION.
Fig. 3A. Cleaning of the restoration prior to luting with water steam cleaner.
Fig. 3B. Marking of the bonding surface as an visual aid for the air-abrasion.
Fig. 3C. Air-abrasion with 50-μm Al2O3 particles with 1 bar pressure.
Fig. 3D. Application of a primer containing 10-MDP.
Fig. 3E. Application of the composite resin cement.
WHICH RESIN CEMENT SYSTEM TO CHOOSE
Subsequently, the components of the resin cement system are applied. Regarding the selection of the system, it is generally recommended to use a restoration primer or resin cement that contains 10-Methacryloyloxydecyl dihydrogen phosphate (10-MDP)11. In this way, a high-quality chemical bond is established. Among the resin cement systems used in the available long-term clinical studies is PANAVIA™ 21 (Kuraray Noritake Dental Inc.)4-6. Launched in 1993, this anaerobic-curing adhesive resin cement contains several important technologies like the MDP monomer and the Touch Cure Technology found in PANAVIA™ V5, the state-of-the art dual-cure multi-bottle adhesive resin cement system of the company. In order to further improve the bonding performance of this present product, however, the team of developers reviewed the basic composition, updated existing technologies and combined them with completely new ingredients.
Even with PANAVIA™ 21 introduced 30 years ago, high success rates were obtained4-6. The few observed failures were mainly due to chipping of the veneering ceramic or debonding. Sometimes caused by traumatic incidents, the debondings resulted in no further damage and the restorations were simply rebonded using the same cementation system and procedure.
One might expect that with its improved formulation, PANAVIA™ V5 will offer an even stronger and more durable bond than predecessor products, so that it is even better suited for such demanding applications as the resin-bonded fixed dental prosthesis. In a pilot study, this assumption was confirmed7. Without any preparation of the abutment tooth, but a defined size of the bonding surface of at least 35 mm2, the team of researchers placed 24 monolithic zirconia resin-bonded bridges (made of KATANA™ Zirconia HT) to replace congenitally missing lateral incisors. The palatal sides of the central incisors were cleaned with pumice paste and treated with phosphoric acid, while the bonding surfaces of the restorations were sandblasted with aluminum oxide particles (50 μm, 2.5 bar pressure). Afterwards, twelve restorations were luted with PANAVIA™ V5, the other twelve with PANAVIA™ F2.0 (another earlier-version resin cement from Kuraray Noritake Dental Inc.). After an observation period of 32 to 50.47 months, the success and survival rates in the PANAVIA™ V5 group were 100 percent. In the other group, a connector fracture, a chipping and two debondings occurred. Based on these results, the authors of the publication concluded that “it has been seen that the new generation cement (PANAVIA™ V5) is more successful”7.
CONCLUSION
For many years, minimally invasive indirect restorative approaches like the replacement of missing incisors with resin-bonded fixed dental prostheses have been performed successfully by some dental practitioners. Many others, however, still seem to be hesitant whether these approaches will lead to the desired results in their hands. The available clinical study results, however, have confirmed that the procedure is highly advantageous and successful, while ongoing development efforts in the field of adhesive resin cements have led to products further decreasing the failure rates related to debonding. Even if a debonding occurs, however, no damage is usually done, so that the restoration can be rebonded again with little effort. These findings – together with the well-known benefits of minimally invasive dentistry in general – should encourage dental practitioners to start exploring the full potential of adhesive dentistry for themselves. In this context, PANAVIA™ V5 is definitely an excellent choice.
References
1. Sasse M, Kern M. All-ceramic resin-bonded fixed dental prostheses: treatment planning, clinical procedures, and outcome. Quintessence Int. 2014 Apr;45(4):291-7. doi: 10.3290/j.qi.a31328. PMID: 24570997.
2. Tetsch J, Spilker L, Mohrhardt S, Terheyden H (2020) Implant Therapy for Solitary and Multiple Dental Ageneses. Int J Dent Oral Health 6(6): dx.doi. org/10.16966/2378-7090.332.
3. Wei YR, Wang XD, Zhang Q, Li XX, Blatz MB, Jian YT, Zhao K. Clinical performance of anterior resin-bonded fixed dental prostheses with different framework designs: A systematic review and meta-analysis. J Dent. 2016 Apr;47:1-7. doi: 10.1016/j.jdent.2016.02.003. Epub 2016 Feb 11. PMID: 26875611.
4. Kern M, Passia N, Sasse M, Yazigi C. Ten-year outcome of zirconia ceramic cantilever resin-bonded fixed dental prostheses and the influence of the reasons for missing incisors. J Dent. 2017 Oct;65:51-55. doi: 10.1016/j.jdent.2017.07.003. Epub 2017 Jul 5. PMID: 28688950.
5. Kern M. Fifteen-year survival of anterior all-ceramic cantilever resin-bonded fixed dental prostheses. J Dent. 2017 Jan;56:133-135.
6. Sasse M, Kern M. Survival of anterior cantilevered all-ceramic resin-bonded fixed dental prostheses made from zirconia ceramic. J Dent. 2014 Jun;42(6):660-3. doi: 10.1016/j.jdent.2014.02.021. Epub 2014 Mar 5. PMID: 24613605.
7. Bilir H, Yuzbasioglu E, Sayar G, Kilinc DD, Bag HGG, Özcan M. CAD/CAM single-retainer monolithic zirconia ceramic resin-bonded fixed partial dentures bonded with two different resin cements: Up to 40 months clinical results of a randomized-controlled pilot study. J Esthet Restor Dent. 2022 Oct;34(7):1122-1131. doi: 10.1111/jerd.12945. Epub 2022 Aug 3. PMID: 35920051.
8. Kern M. Bonding to oxide ceramics—laboratory testing versus clinical outcome. Dent Mater. 2015 Jan;31(1):8-14. doi: 10.1016/j.dental.2014.06.007. Epub 2014 Jul 21. PMID: 25059831.
9. Kern M, Beuer F, Frankenberger R, Kohal RJ, Kunzelmann KH, Mehl A, Pospiech P, Reis B. All-ceramics at a glance. An introduction to the indications, material selection, preparation and insertion techniques for all-ceramic restorations. Arbeitsgemeinschaft für Keramik in der Zahnheilkunde. 3rd English edition, January 2017.
10. Comino-Garayoa R, Peláez J, Tobar C, Rodríguez V, Suárez MJ. Adhesion to Zirconia: A Systematic Review of Surface Pretreatments and Resin Cements. Materials (Basel). 2021 May 22;14(11):2751.
11. Al-Bermani ASA, Quigley NP, Ha WN. Do zirconia single-retainer resin-bonded fixed dental prostheses present a viable treatment option for the replacement of missing anterior teeth? A systematic review and meta-analysis. J Prosthet Dent. 2021 Dec 7:S0022-3913(21)00588-6. doi: 10.1016/j.prosdent.2021.10.015. Epub ahead of print. PMID: 34893319.