BEST.FIT: A hybrid technique for an efficient and aesthetic restoration of anterior teeth
Case by Dr. Enzo Attanasio
The introduction of new-generation composites, equipped with nanofillers and highly loaded, has opened doors to new techniques for managing direct and semi-direct restorations. In particular, over the last ten years, there has been a significant revolution in the world of flowable composites. Nowadays, these materials offer a filler percentage very similar to packable composites through precise interventions in resin matrix management. They come in various viscosities, offering numerous advantages both in terms of handling and clinical use, as well as beneficial mechanical and physical characteristics.
FLOWABLE INJECTION TECHNIQUE
This new era of flowable composites has seen the development of a technique known as the Flowable Injection Technique (also referred to as injection moulding). It enables dental practitioners to reproduce anatomical forms created by a dental technician in the laboratory through a diagnostic wax-up. The shapes planned on the model are transferred directly in the patient's mouth using transparent silicone matrices or indexes, into which the composite is injected through specific injection holes.
The main difference compared to traditional mock-ups is that the reproduced dental elements remain separate from each other. This technique provides predictable results identical to those developed on the technician's wax-up, requiring less chair time than direct veneering and offering a longevity similar to traditional composite restorations.
BENEFITS AND CHALLENGES
The major benefit of this technique is the faithful reproduction of morphological details that the technician creates on the diagnostic wax-up, which the clinician can reproduce with minimal effort. The restoration produced through the flowable injection technique, if all steps are followed correctly, requires minimal finishing by the clinican, who only needs to focus on polishing the composite.
However, one limitation is the difficulty in isolating the operative field, often requiring a split-dam technique or labial retractors, with all the associated adhesive challenges. The use of a rubber dam is only feasible if the peripheral dental tissues around the restoration are euchromatic, allowing the technician to create a wax-up with supragingival preparation margins.
Another compromise with the flowable injection technique is the management of the composite as a single mass. This makes it only possible to reproduce natural incisal translucencies typical of young patients by performing complex cutbacks and subsequent incisal painting. Without specific operator skills, the outcomes of this time-consuming manual procedure are unpredictable.
HYBRID TECHNIQUE: BEST.FIT
To leverage the advantages of both classical direct anterior restoration and flowable injection techniques and eliminate the limitations, a hybrid technique known as BEST.FIT (Buccal Enamel Shade Through Flow Injection Technique) has emerged. This technique allows the operator to manage the delicate phase of reproducing the buccal enamel layer of the anterior restoration through the flowable injection technique, keeping certain aspects in mind during the injection phase.
PROCEDURE
The transparent silicone key used for the creation of the buccal enamel layer is similar to the one used in the original flowable injection technique. The initial phase of restoration management follows all the classical steps of direct technique, requiring isolation with rubber dam. The palatal enamel layer is recreated with a highly translucent packable composite, and the palatal portion of the interproximal walls is produced using a suitable matrix system. Then, the core of the restoration is defined with opaque masses, creating mamelons and adding incisal effects. It's crucial to control the residual enamel thickness using a vestibular silicone index, aiming for about 0.3 mm of space. The buccal portion is finally reconstructed during the injection phase. The transparent silicone index created on the wax-up should be tested after each reconstruction phase to ensure passive insertion.
After creating the restoration core, the element to be injected is separated from the contiguous ones with thin PTFE tape. The transparent mask is then inserted, and fluid composite is injected through the injection holes to precisely reconstruct the buccal enamel thickness. The composite tip should be positioned at least halfway through the buccal surface, and the injection should be slow and controlled to avoid air bubbles in the material.
FINISHING
Following a 40-second polymerization vestibularly and occlusally, the transparent matrix is carefully removed, and excess interproximal composite above the PTFE tape as well as any remaining composite cylinder from the injection holes are removed. After completing all restorative elements, the rubber dam is dismantled, and composite excess is finished. After checking the occlusion, the composite is polished, usually requiring no further intervention.
CASE EXAMPLE
Fig. 1. Female patient with discoloured anterior restorations desiring a smile makeover.
Fig. 2. Close-up of her maxillary anterior teeth.
Fig. 3. Restorations in need of replacement: Lateral view from the right.
Fig. 4. Restorations in need of replacement: Lateral view from the left.
Fig. 5. Printed model based on a digital diagnostic wax-up based on a digital impression.
Fig. 6. Palatal silicone index produced for the conventional direct restoration steps.
Fig. 7. Transparent matrix with injection holes produced for the build-up of the buccal enamel layer using the flowable injection technique.
Fig. 8. Operative field isolated with rubber dam.
Fig. 9. Existing restorations removed and tooth surfaces roughened at the start of treatment.
Fig. 10. Palatal silicone index positioned intraorally for the build-up of the palatal wall.
Fig. 11. Checking of the space available in the vestibular area with a second silicone index.
Fig. 12. Etching with phosphoric acid etchant.
Fig. 13. Application of a universal adhesive (CLEARFIL™ Universal Bond Quick, Kuraray Noritake Dental Inc.).
Fig. 14. Palatal walls built up with CLEARFIL MAJESTY™ ES-2 Premium in the shade A1E with the aid of the palatal silicone index.
Fig. 15. Build-up of the interproximal walls with CLEARFIL MAJESTY™ ES-2 Premium in the shade A1D and establishing of the contact points using anatomical sectional matrices for the posterior area placed vertically.
Fig. 16. Dentin core built up with CLEARFIL MAJESTY™ ES-2 Premium in the shade A2D. CLEARFIL MAJESTY™ ES Flow Super Low in the shade XW was applied on the mamelons, while CHROMA ZONE™ COLOR STAIN Blue (Kuraray Noritake Dental Inc.) was used to reproduce incisal translucencies in the spaces not covered by the dentin core.
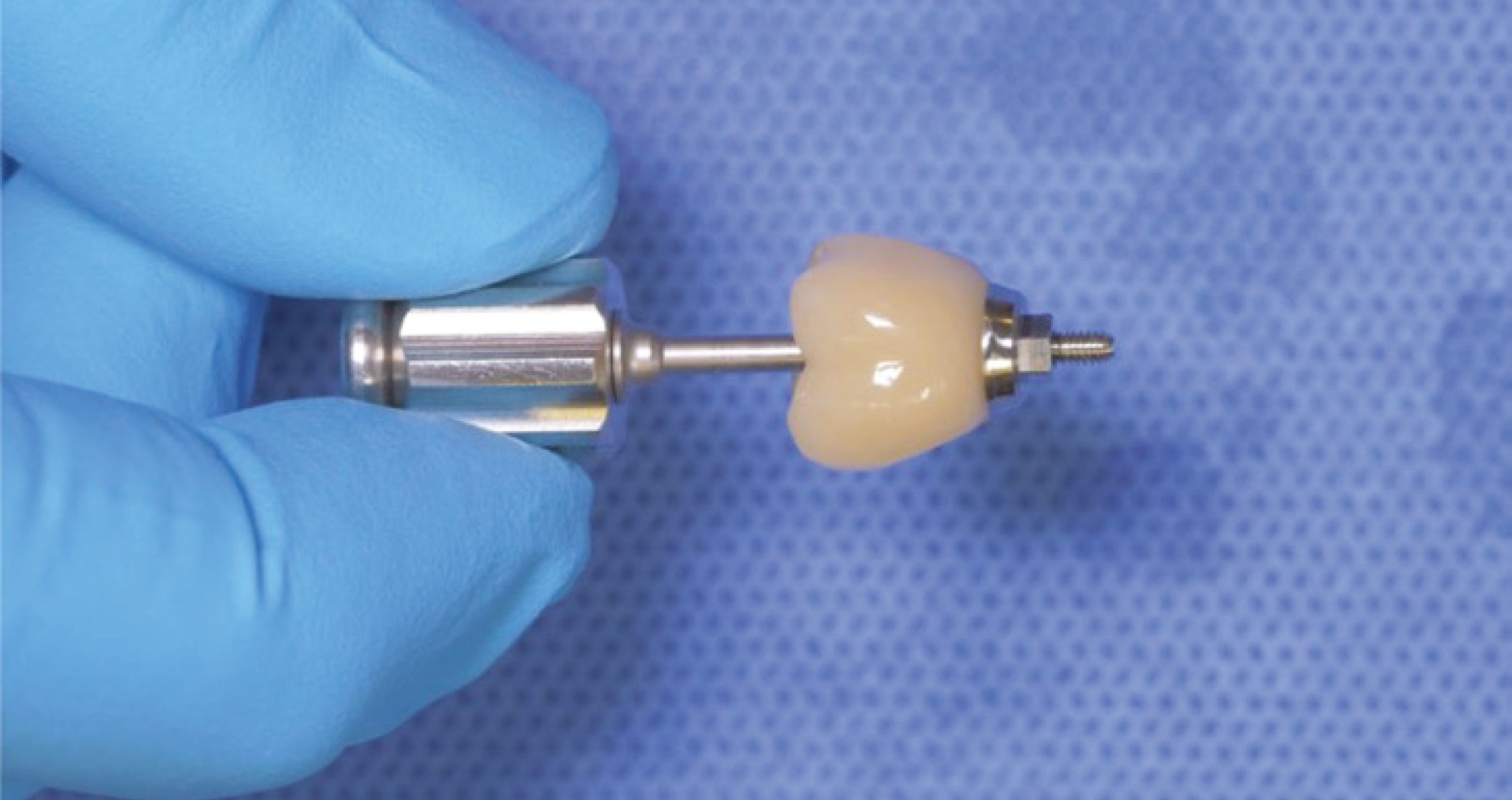
Fig. 17. Try-in of the transparent matrix for flowable injection.
Fig. 18. Isolation of the adjacent teeth with PTFE tape for a one-by-one injection.
Fig. 19. CLEARFIL MAJESTY™ ES FLOW Low in the shade A2 (Kuraray Noritake Dental Inc.) injected for the anatomical shaping of the maxillary right central incisor.
Fig. 20. Situation after flowable injection for all four anterior teeth, light curing through the matrix, final matrix removal and excess removal.
Fig. 21. Treatment outcome …
Fig. 22. … with visible mamelons, natural incisal translucencies …
Fig. 23. … and a lifelike anatomical shape …
Fig. 24. … of the restorations.
CONCLUSION
Each work phase must be executed with extreme care to lay the foundations for a passive linking of all subsequent steps without creating difficult management situations. The BEST.FIT technique is a convenient and useful method for dental practitioners to manage multiple direct anterior restorations simply and predictably, especially in situations requiring complex rehabilitations with large restorations.
Dentist:
ENZO ATTANASIO
Enzo Attanasio graduated in 2008 in Dentistry and Dental Prosthetics from the Magna Graecia University of Catanzaro. In 2009, he went on to specialize in the use of laser and new technologies in the treatment of oral and perioral tissues at the University of Florence. That year he also attended Prof. Arnaldo Castellucci’s course in Clinical Endodontics at the Teaching Center of Microendodontics in Florence where, in 2012, he went on to complete his training in Surgical Microendodontics. In 2017 he attended a course on Direct and indirect Adhesive Restorations at Prof. Riccardo Becciani’s Think Adhesive training center in Florence where he later become a tutor. Today, as a member of the Italian AIC and based in Lamezia Terme, Italy, Dr Attanasio has a special interest in Endodontics and Aesthetic Conservative.